KEY TAKEAWAYS
- The study examined ThINKK cell identity, allogeneic T cell activation, and drug effects on ThINKK-NK interaction.
- The study findings supported ThINKK immunotherapy safety and efficacy, warranting phase I clinical trial advancement.
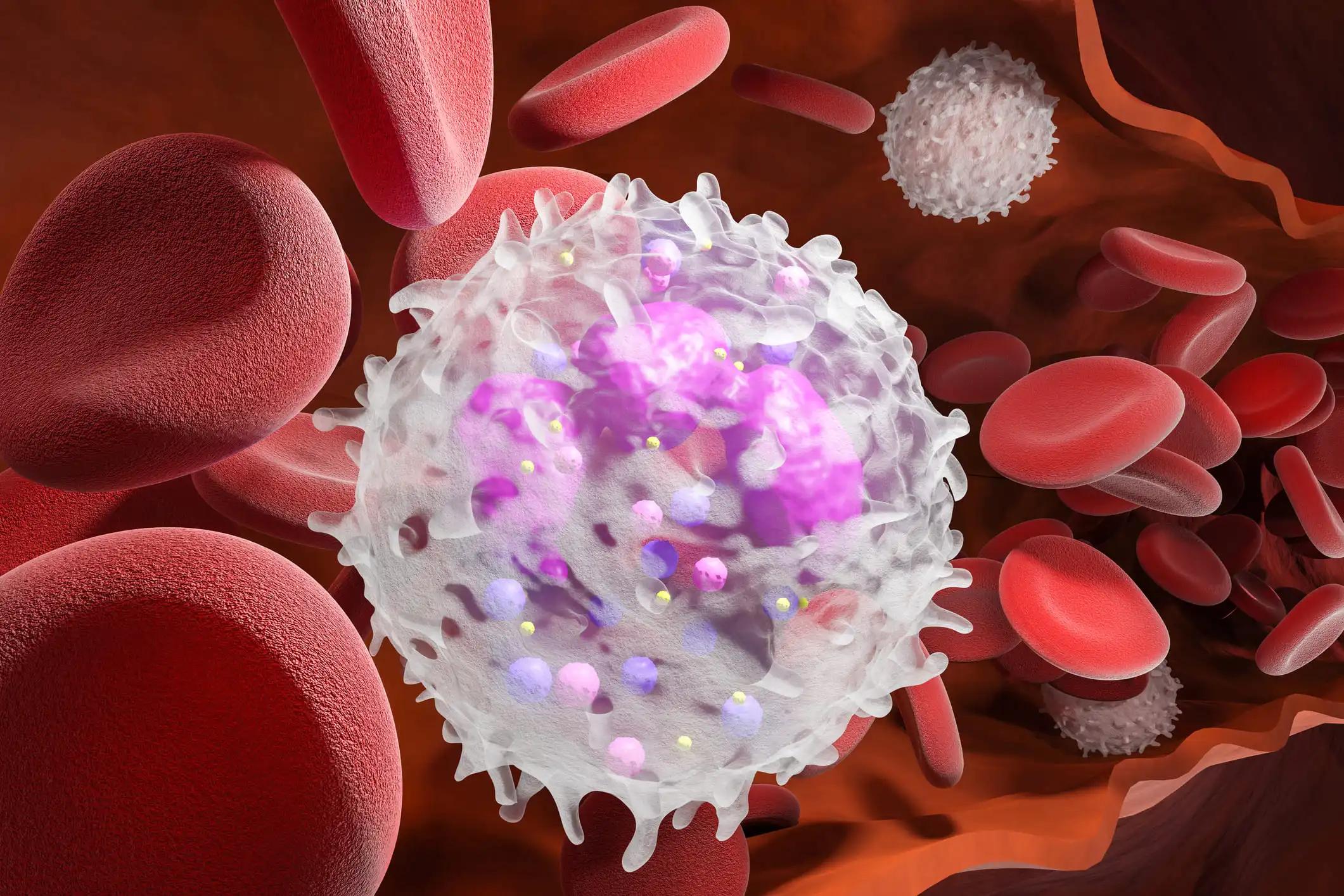
In the treatment of chemotherapy-refractory patients with leukemia, allogeneic hematopoietic stem cell transplantation (HSCT) remains standard, but cure rates are low. Researchers aim to enhance the early graft-versus-leukemia effect post-HSCT by improving natural killer (NK) cell activity. Their approach involves the adoptive transfer of Therapeutic Inducers of Natural Killer cell Killing (ThINKK) derived from expanded and differentiated HSC with blood plasmacytoid dendritic cell (pDC) characteristics.
Previous studies have shown that ThINKK can stimulate NK cells and control the progression of acute lymphoblastic leukemia (ALL) in preclinical mouse models of HSCT for ALL.
Nicolas Poirier and the team aimed to examine the cellular identity of ThINKK cells and explored their ability to activate allogeneic T cells. Additionally, they assessed the impact of immunosuppressive drugs on the interaction between ThINKK and NK cells.
The study explored ThINKK cellular identity through single-cell RNA sequencing and flow cytometry. It investigated its potential to activate allogeneic T cells by coculturing them with antigen-presenting cells, with or without ThINKK. A preclinical human-to-mouse xenograft model assessed the impact of ThINKK injections on graft-versus-host disease (GvHD). It tested the effect of immunosuppressive drugs on ThINKK-induced NK cell cytotoxicity against ALL cells.
Most ThINKK exhibited key characteristics similar to canonical blood pDC, notably robust type-I interferon (IFN) production when stimulated by Toll-like receptors. A smaller subset expressed some markers of other dendritic cell populations, though not all. ThINKK were resistant to killing by allogeneic T or NK cells and did not enhance T cell proliferation induced by antigen-presenting cells or exacerbate GvHD in vivo. Furthermore, tacrolimus, sirolimus, or mycophenolate did not diminish ThINKK-induced NK cell activation and cytotoxicity.
The study concluded that ThINKK cells, characterized by type I interferon production and limited T cell activation, are unlikely to increase the risk of GvHD post-allogeneic HSCT. Additionally, using tacrolimus, sirolimus, or mycophenolate as anti-GvHD prophylaxis is predicted not to compromise ThINKK therapeutic effectiveness. These preclinical findings collectively supported the advancement of ThINKK immunotherapy into phase I clinical trials.
Funding was provided by the Foundation Charles Bruneau, BioCanRx Network, and Canadian Institute of Health Research grants.
Source: https://pubmed.ncbi.nlm.nih.gov/38754915/
Poirier N, Paquin V, Leclerc S, et al. (2024). “Therapeutic Inducers of Natural Killer cell Killing (ThINKK): preclinical assessment of safety and efficacy in allogeneic hematopoietic stem cell transplant settings.” J Immunother Cancer. 2024 May 15;12(5):e008435. doi: 10.1136/jitc-2023-008435. PMID: 38754915.