KEY TAKEAWAYS
- The study was a phase 2, BAITP trial aimed at investigating the efficacy and tolerability of baricitinib as a second-line treatment for patients with steroid-resistant or recurrent ITP.
- The modified intention-to-treat population was analyzed, including all enrolled patients except those who withdrew consent or did not meet the eligibility criteria.
- The study found that 71.4% of patients exhibited a durable response to baricitinib treatment, and 64.3% exhibited an initial response.
- About 22 patients (78.6%) received concomitant medications at baseline, including corticosteroids (50%) and TPO-RAs (42.9%).
- The daily dose of 4 mg baricitinib was well tolerated and showed potential effectiveness in treating steroid-resistant or recurrent ITP.
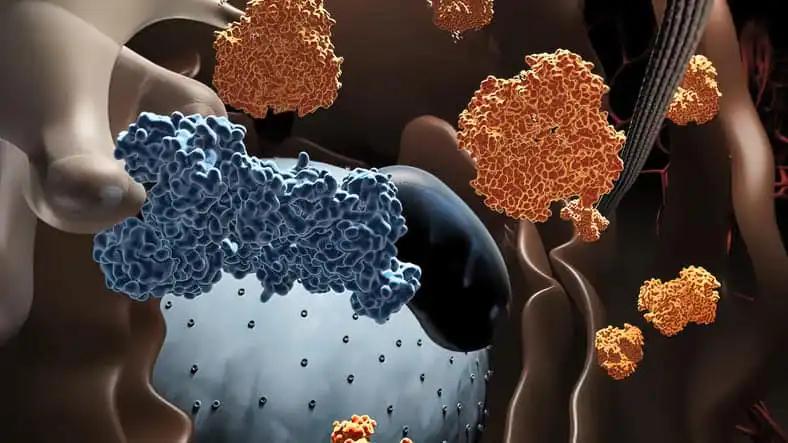
Immune thrombocytopenia (ITP) patients with steroid resistance or relapse have an increased risk of bleeding and impaired quality of life. Multiple cytokine signaling pathways involved in self-reactive innate and adaptive immune responses are modulated by baricitinib, a selective and reversible inhibitor of Janus-associated kinase 1 (JAK1) and JAK2. To maintain the self-reactive adaptive immune response, splenic macrophages phagocytose IgG-opsonized platelets and present the internalized platelet antigens to activate T and B cells. Baricitinib reduces B-cell abnormalities and antibody production by inhibiting IFN-induced antigen presentation by innate immune cells and subsequent T-cell activation. Baricitinib may therefore ameliorate both innate and adaptive immune disorders in ITP.
This phase 2 trial with a single limb and an open-label was conducted at the Peking University People’s Hospital. This study was available to adult patients with steroid-resistant or recurrent ITP and a platelet count of 30×109/L or 50×109/L with clinically significant bleeding. Patients received 4 mg of baricitinib daily for six months.
The primary outcome measure was response stability at the 6-month follow-up. The modified intention-to-treat population included all enrolled patients except those who withdrew consent or post hoc did not objectively meet the eligibility criteria (e.g., a diagnosis of secondary ITP after enrollment, de novo infections, or laboratory abnormalities before baricitinib administration). The safety profiles of patients who received at least one dose of baricitinib were analyzed (NCT05446831). This study is registered with ClinicalTrials.gov. A total of 35 patients were enrolled, with 28 comprising the modified intention-to-treat population. About 20 patients exhibited a durable response (71.4%, 95% CI, 51.3 to 86.8), and 18 patients demonstrated an initial response (64.3%). About 13 days (IQR: 6.75–22.5) elapsed between the initial treatment and the response onset. Since the 4-week follow-up, patients receiving baricitinib had a median platelet count of < 50 ×109/L, which remained stable at 72-81×109/L throughout the treatment period.
At baseline, 22 patients (78.6%) received concomitant medications, including corticosteroids (14/28, 50%) and TPO-RAs (12/28, 42.9%). Some patients who responded to treatment were tapered off or discontinued from these medications. At the most recent visit, 12 patients (42.9%) were receiving concomitant medications, including three patients (10.7%) receiving corticosteroids and seven patients (25.0%) receiving TPO-RAs. As measured by the Primary ITP-Patient Assessment Questionnaire (ITP-PAQ) scales, patients receiving baricitinib reported improved quality of life. Infections were the most prevalent adverse events (6/28, or 21.4%). In 1 (3.6%) patients, treatment discontinuation owing to an adverse event was reported. It is the first study to describe JAK inhibition as an ITP treatment. The daily dose of 4 mg baricitinib was well tolerated and may be effective in treating steroid-resistant or recurrent ITP. This result may contribute to refining second-line therapy for ITP, and further randomized, controlled trials are warranted.
Source: https://library.ehaweb.org/eha/2023/eha2023-congress/386041/peng.zhao.baricitinib.for.steroid-resistant.relapse.immune.thrombocytopenia.html?f=menu%3D16%2Abrowseby%3D8%2Asortby%3D2%2Ace_id%3D2489%2Aot_id%3D27904%2Atrend%3D4016%2Amarker%3D4178
Clinical Trial: https://classic.clinicaltrials.gov/ct2/show/NCT05446831
Peng Zhao, Zhuo-yu An, Hai-xia Fu, Hui-xin Liu, Qiu-sha Huang, Li-ping Yang, Qing-yuan Qu, Jin Wu, Ye-jun Wu, Yu-xiu Chen, Meng-lin Li, Chencong Wang, Xiaolu Zhu, Yun He, Juan-juan Li, Yuan-yuan Zhang, Qian Jiang, Hao Jiang, Jin Lu, Ying-jun Chang, Xiao-su Zhao, Xiang-yu Zhao, Xiao-jun Huang, Xiao-Hui Zhang/BARICITINIB FOR STEROID-RESISTANT/RELAPSE IMMUNE THROMBOCYTOPENIA (BAITP): AN OPEN-LABEL, SINGLE-ARM, PHASE 2 TRIAL/Inc, M. G. (n.d.). BARICITINIB FOR STEROID-RESISTANT/RELAPSE IMMUNE THROMBOCYTOPENIA… by Peng Zhao. Library.ehaweb.org. Retrieved July 14, 2023, from https://library.ehaweb.org/eha/2023/eha2023-congress/386041/peng.zhao.baricitinib.for.steroid-resistant.relapse.immune.thrombocytopenia.html?f=menu%3D16%2Abrowseby%3D8%2Asortby%3D2%2Ace_id%3D2489%2Aot_id%3D27904%2Atrend%3D4016%2Amarker%3D4178