KEY TAKEAWAYS
- This ongoing phase 1 and 2 TACTIC-2 clinical trial assesses the safety and initial anti-tumor activity of TAC01-HER2 in treating HER2+ solid neoplasms.
- The study suggests that TAC01-HER2 is safe and effective in a heavily pre-treated cancer population, refractory to prior HER2-targeted treatments.
- The dose escalation study of TAC01-HER2 continues to understand its full therapeutic potential and safety profile.
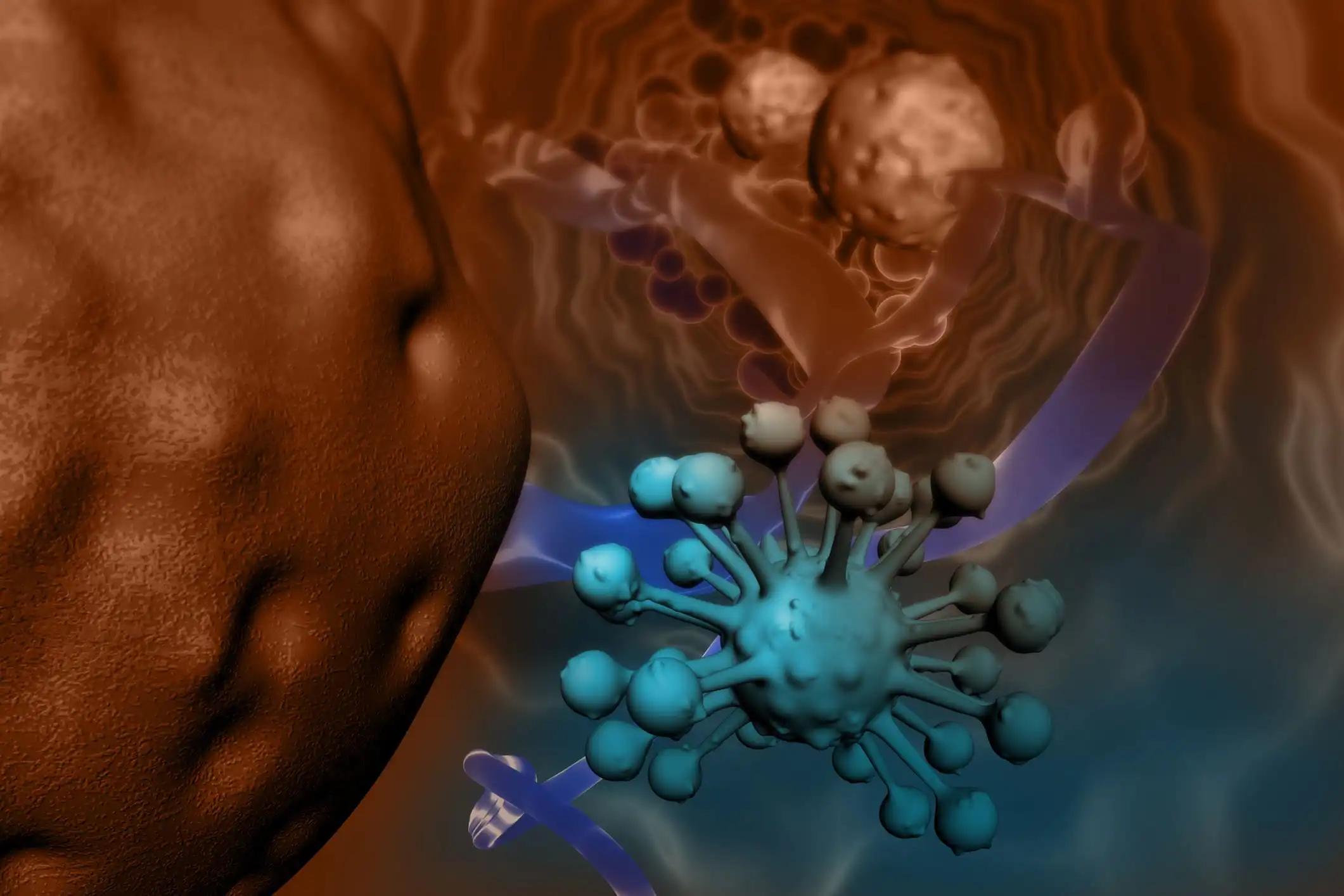
Despite advancements in therapies for advanced or metastatic HER2-positive (HER2+) solid tumors, there remains a substantial gap in addressing the medical needs of these patients (pts). The T cell antigen coupler (TAC) technology is an innovative methodology that modifies T cells ex vivo, facilitating them to detect and exert cytotoxic actions on solid tumor cells by utilizing the intrinsic T cell receptor. TAC-activated T cells demonstrate more reliable anti-tumor responses than chimeric antigen receptor T cells. TAC01-HER2 represents an autologous T-cell therapeutic comprised of T cells expressing the HER2 TAC. Preclinical murine studies revealed that TAC01-HER2 induced tumor regression or eradication in models resistant to other HER2-targeted treatments without any associated TAC toxicities.
The ongoing clinical trial has been assessing the safety and initial anti-tumor activity of TAC01-HER2 in treating HER2+ solid neoplasms. Participants undergo leukapheresis and subsequent bridging therapy (if required) during the manufacturing of TAC01-HER2 cells and undergo lymphodepletion chemotherapy (LDC) prior to TAC01-HER2 infusion. In the phase I dose escalation, the primary endpoint is determining the safety profile of TAC01-HER2 at escalating doses of 0.3, 0.8, 3, and 8 x 10ˆ6 cells/kg (Cohorts 1-4, respectively) in adults with HER2+ solid tumors who have advanced after receiving ≥2 systemic therapy lines. Dose-limiting toxicities (DLTs) are monitored for 28 days post-TAC01-HER2 infusion. Phase II will further explore the safety, efficacy, and pharmacokinetics of the recommended TAC01-HER2 dose in HER2+ solid tumors.
As of February 21, 2023, 18 pts with solid tumors were administered treatment in Cohorts 1-4, with 3 of them being HER2-low. All displayed TAC transgene presence in blood, and it was found in the tumor region of one patient in Cohort 4. A single DLT instance of grade 3 pneumonitis was noted in Cohort 4. Neurotoxicity was absent. Most Cohorts 3 and 4 patients presented with Grade ≤2 CRS, managed through supportive care. Twelve patients reported 21 severe adverse incidents. Of these, 17 were not associated with TAC01-HER2, but there were exceptions: one event of Grade 3 pneumonitis, one of Grade 1, and two of Grade 2 CRS. Most of these adverse events were attributed to LDC or the underlying malignancy.
A disease control rate of 64% was noted in Cohorts 2-4, four weeks post TAC01-HER2 administration. Two pts exhibited an unconfirmed partial response (PR), whereas 12 demonstrated a stable condition. In Cohort 4, a patient with refractory metastatic GEJ adenocarcinoma (HER2 2+, FISH positive) showed an unconfirmed PR upon the 4-week restaging, completely reducing the targeted lesion. This patient had progressed on four different therapeutic approaches, including treatments with trastuzumab and trastuzumab deruxtecan. The second unconfirmed PR identified in Cohort 2 showed a 35% decrease in target lesions.
The TAC01-HER2 T cell therapy demonstrates a manageable safety profile and notable clinical efficacy in a cohort extensively pre-treated for cancer and resistant to prior HER2-centric treatments. The dose escalation study of TAC01-HER2 remains in progress.
Source: https://www.annalsofoncology.org/article/S0923-7534(23)00229-6/fulltext
Clinical Trial: https://classic.clinicaltrials.gov/ct2/show/NCT04727151
Dumbrava, E., Olson, D., George, M., Saibil, S., Antonio, G., Bouvier, R., Gavriliuc, M., Pieke, B., Lichtenstein, E., Geisberger, J., Apostolopoulou, M., Moss, K., Ternus, N., Adib, D., Schlechter, B. A PHASE I/II TRIAL INVESTIGATING SAFETY AND EFFICACY OF AUTOLOGOUS TAC01-HER2 IN RELAPSED OR REFRACTORY SOLID TUMORS. https://doi.org/10.1016/j.annonc.2023.04.087