KEY TAKEAWAYS
- The phase 3 REACH-3 study assessed the safety and effectiveness of ruxolitinib in pts who crossed over from the best available treatment.
- The study suggested that patients who crossed over from BAT to ruxolitinib experienced high response rates with no new safety concerns.
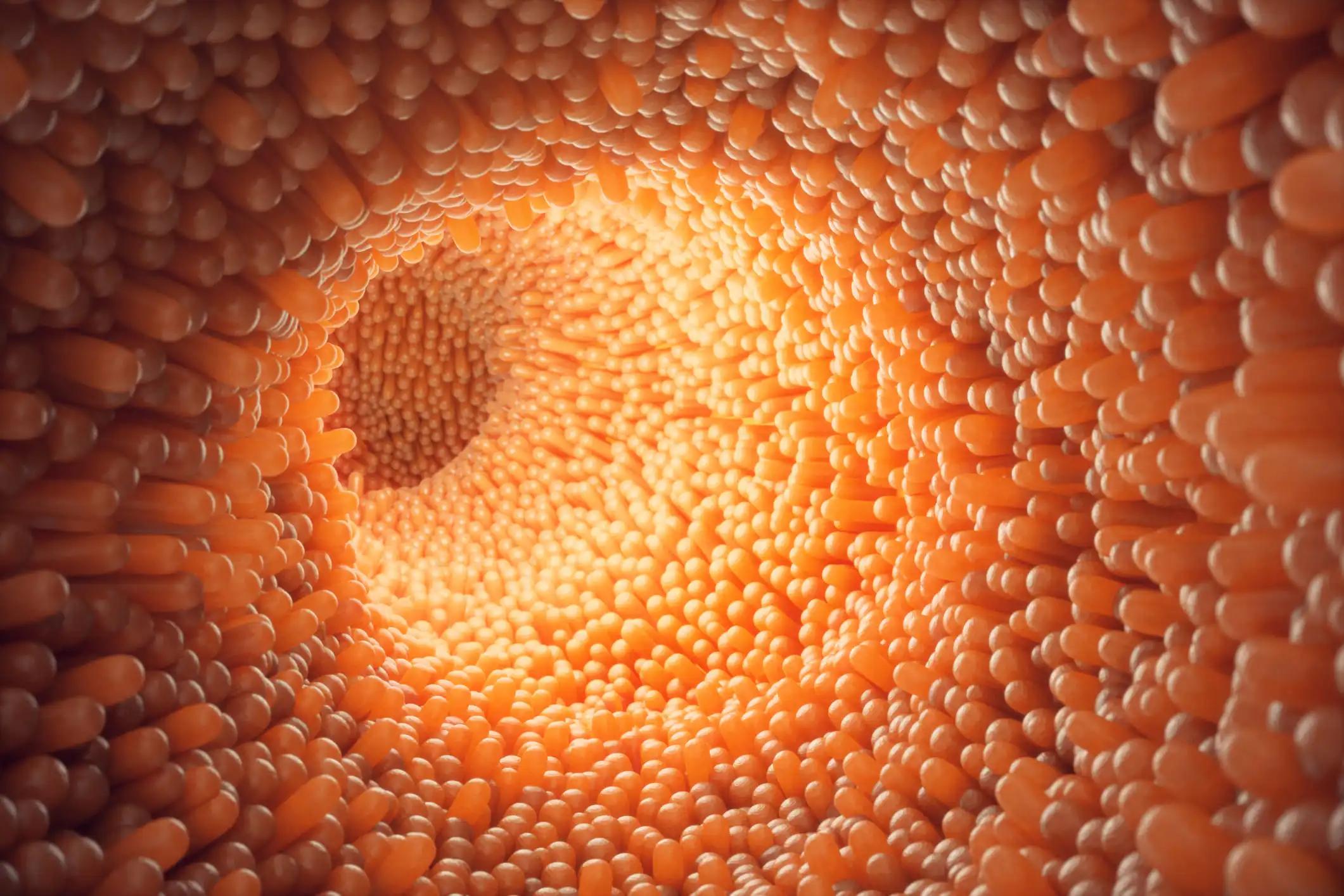
A serious complication observed in 30–70% of allogeneic stem cell transplant recipients is Chronic graft-versus-host disease (cGvHD). Though glucocorticoids are the standard initial treatment, about half of the patients (pts) either become non-responsive or dependent on them, leading to poorer outcomes. Ruxolitinib, a drug designed to selectively inhibit JAK1/2, has been recently approved in the US and Europe for treating such pts based on the findings of the REACH-3 clinical trial.
In this study, ruxolitinib showcased a higher overall response rate, best overall response, and extended duration of response when compared to the best available treatment. Researchers further assessed the safety and effectiveness of ruxolitinib in pts who crossed over from BAT.
The REACH-3 study randomized pts 12 years or older with cGVHD who didn’t respond well to the usual treatment to either get ruxolitinib (165 participants) or another best available treatment (164 participants). After 24 weeks, pts on the best available treatment could switch to ruxolitinib if they didn’t show adequate response, experienced a cGVHD relapse, or had adverse effects.
Of the pts, 69 (or 42.1%) transitioned to ruxolitinib. As of June 25, 2021, two completed their treatment, and 34 were still on it. Those who quit ruxolitinib before the 24-week mark were labeled as non-responders. 33 pts (or 47.8%) stopped ruxolitinib, mainly due to the doctor’s advice, lack of effectiveness, or the decision of the patient or their guardian. 22 pts (31.9%) entered a long-term survival monitoring phase.
At the 24-week mark post-transition, the overall response rate stood at 47.8%. Three pts (4.3%) showed a complete response, and 30 (or 43.5%) displayed a partial response. The best response noted during this crossover period was 79.7%, which aligns with the initial study’s findings.
The average duration of ruxolitinib use post-transition was 75.7 weeks. Even with extended use, its safety profile remained consistent with previous observations. Common side effects included anemia, upper respiratory tract infections, cough, and fever. Out of the lot, 6 pts (8.7%) passed away, primarily from infections, while one death was due to cGVHD.
Patients who crossed over from BAT to ruxolitinib experienced high response rates. The ORR and BOR results matched the observations made during the initial randomized trial. There were no new safety concerns identified among the crossover pts. These results further endorse ruxolitinib as an effective option for SR/D cGVHD pts who haven’t benefited from other treatments.
Source: https://ebmt2023.abstractserver.com/program/#/details/presentations/1693
Clinical Trial: https://classic.clinicaltrials.gov/ct2/show/NCT03112603
Russo, D., Locatelli, F., Teshima, T., Lee, S.J., Li, X., Stefanelli, T., Gowda, M., Zeiser, R. OS05-01 EFFICACY AND SAFETY OF RUXOLITINIB IN PATIENTS WITH STEROID-REFRACTORY CHRONIC GRAFT VERSUS HOST DISEASE AFTER CROSSOVER IN THE PHASE 3 REACH-3 STUDY.