KEY TAKEAWAYS
- The phase II trial assessed the safety and efficacy of trilaciclib in patients receiving SG for mTNBC.
- The study’s endpoints included antitumor efficacy, myeloprotection, and safety/tolerability.
- Preliminary data indicated trilaciclib before SG may reduce multiple AEs compared to SG alone trials.
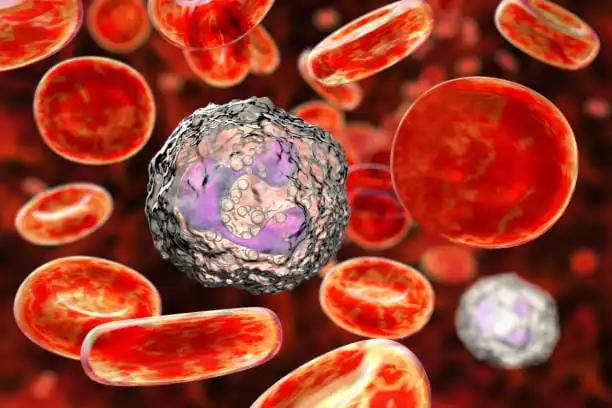
Trilaciclib, in a phase II trial for metastatic triple-negative breast cancer (mTNBC) patients (pts), demonstrated its ability to protect hematopoietic stem and progenitor cells that rely on CDK4/6 during chemotherapy, providing myeloprotection. Meanwhile, SG, an antibody-drug conjugate used to treat mTNBC pts, significantly extended survival in the phase III ASCENT trial compared to single-agent chemotherapy. It was associated with increased rates of neutropenia (any grade [G], 63% vs. 43%; G3/4, 51% vs. 33%) and diarrhea (any grade [G], 59% vs. 12%; G3/4, 10% vs. <1%).
In a separate phase II trial, trilaciclib demonstrated its ability to modulate antitumor immunity when administered before chemotherapy in mTNBC (Tan et al., Clin Cancer Res, 2022). Given these findings, there is potential for administering trilaciclib before SG treatment to enhance antitumor effectiveness and reduce myelotoxicity in mTNBC pts. This study shared the preliminary safety and efficacy results from a phase II, single-arm trial of trilaciclib in pts receiving SG for mTNBC.
Adult pts who meet the following criteria (having received ≥ prior systemic therapies, with at least one in a metastatic setting, having measurable disease, confirmed hormone receptor-/HER2-negative, and having an ECOG PS 0/1) were eligible for this study. These eligible pts were administered intravenous trilaciclib at 240 mg/m2 before receiving SG at 10 mg/kg on Days 1 and 8 of each 21-day cycle. This treatment regimen continues until either disease progression or the development of unacceptable toxicity. Tumor assessments are conducted at various intervals, including at the initial screening, every 6 weeks up to week 36, and then every 9 weeks until disease progression or subsequent anticancer therapy. The study’s endpoints were antitumor efficacy, myeloprotection, and safety/tolerability of the treatment.
As of January 17, 2023, 26 out of the planned 45 female pts had been enrolled and had completed a median number of 4 cycles, ranging from 2 to 15. These pts had previously undergone a median of 2 treatment lines, ranging from 2 to 5, including treatments with taxanes in 20 cases and immune checkpoint inhibitors in 18 cases. The study will present the objective response rate based on the PD-L1 status. One patient experienced adverse events (AEs) that led to the study drugs’ discontinuation.
Preliminary data indicated that administering trilaciclib before SG treatment may lower the rate and intensity of various AEs compared to trials of SG alone. This warrants further ongoing evaluation.
Clinical Trial: https://classic.clinicaltrials.gov/ct2/show/NCT05113966
Seneviratne, L., Harnden, K.K., Mardones, M., Blau, S., Gillespie-Twardy, A., Danso, M.A., Berz, D., Guaqueta, D., Schwerkoske, J., O’Shaughnessy, J., Patt, D., Bardia, A., Beelen, A., Oyekunle, T., Dell, V., Hurvitz, S.A. 201P – Trilaciclib combined with sacituzumab govitecan (SG) in metastatic triple-negative breast cancer (mTNBC): Preliminary phase 2 results. Annals of Oncology (2023) 8 (1suppl_4): 101223-101223. 10.1016/esmoop/esmoop101223.