KEY TAKEAWAYS
- This study analyzed the safety and efficacy of oral DEC/CED in CMML pts.
- The study’s endpoints were the best response by IWG 2006, TI, TFS, OS, and safety.
- The study showed that DEC/CED is safe and effective in treating CMML pts.
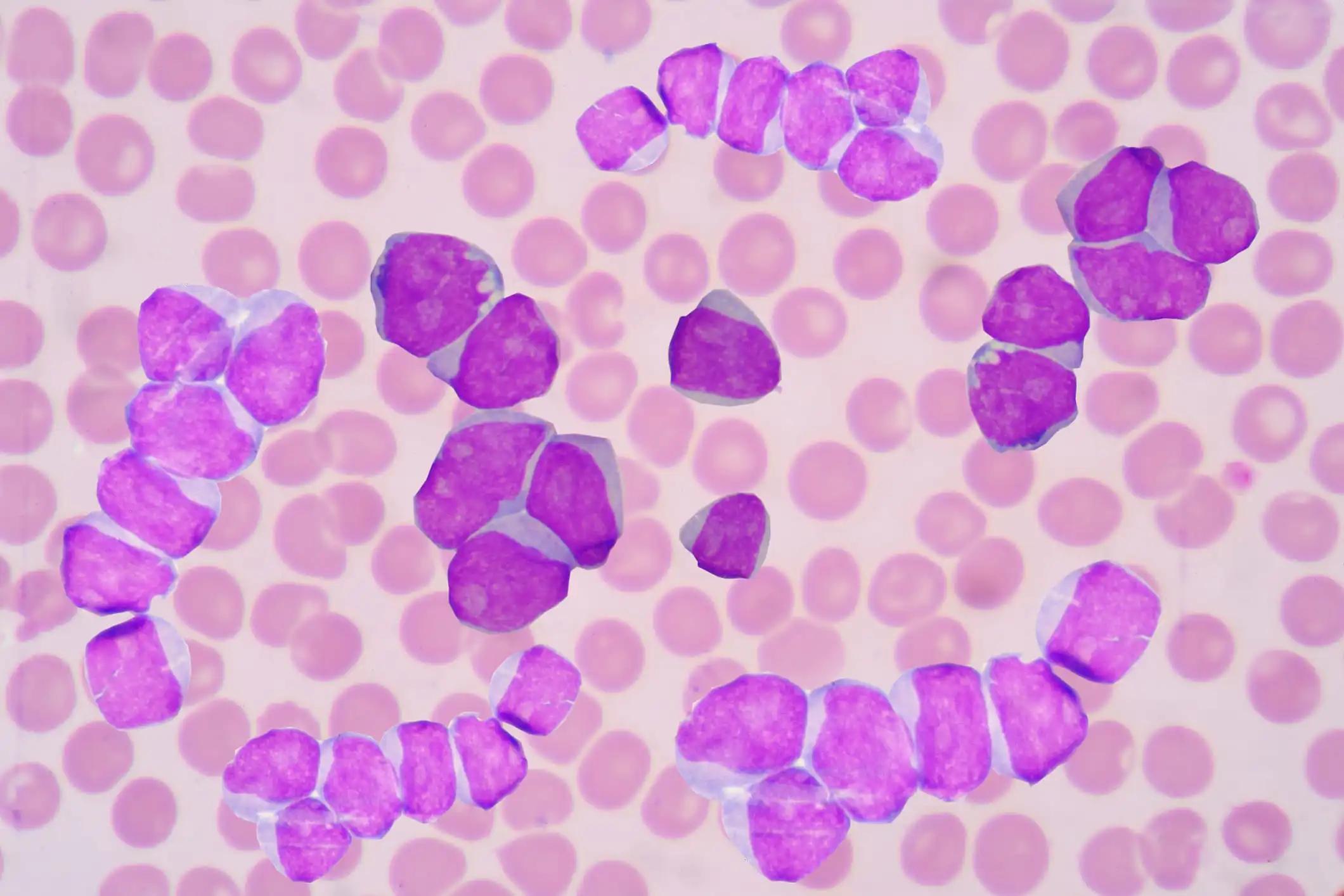
Chronic Myelomonocytic Leukemia (CMML) is a clonal hematopoietic stem cell disease. ASTX727, an orally available fixed-dose combination (FDC) of 35 mg of decitabine (DEC) and 100 mg of cedazuridine (CED)—an inhibitor of cytidine deaminase—has been shown to have a pharmacokinetic area under the curve (PK AUC) similar to that of intravenous DEC, as per a study by Garcia-Manero and colleagues in 2019.
Researchers shared the combined clinical experience of CMML patients (pts) in studies leading to FDA approval of oral DEC/CED. These studies are registered under ClinicalTrials.gov NCT02103478 and NCT03306264 and include information on the patients’ genetic makeup.
The study included 33 CMML pts with PS 0-2. Patients were administered the standard oral DEC/CED regimen. Clinical endpoints were the best response as per the International Working Group (IWG) 2006, transfusion independence (TI), transformation-free survival (TFS), overall survival (OS), and safety. Molecular profiling utilized an NGS panel, which included somatic mutations that could affect CMML prognosis and response to HMA therapy. Cox regression analysis was conducted on various factors to analyze the risk factors for OS.
The pts had a median age of 71, and 55% were assessed with ECOG PS 1. Notably, 85% of the pts had not undergone any previous anticancer treatments for CMML. Around one-third were RBC transfusion-dependent at baseline, 70% were CMML-1, and 76% were MD-CMML. The pts underwent a median of 10 therapy cycles. The pts received a median of 10 therapy cycles (range 2 to 36 cycles).
In the study, 7 pts (21.2%) achieved complete responses (CR), and 14 (42.4%) had marrow complete responses (mCR), of which 5 (15.2%) also showed hematologic improvement (HI). The overall response rate (ORR), which includes CR, partial responses (PR), mCR, and HI, was 75.8%. Among those RBC transfusion-dependent at baseline, 63.6% achieved transfusion independence (TI) for at least eight weeks. The mTFS was 28.3 months, and the mOS was 35.7 months.
Regarding safety, the profile aligned with what is typically seen with decitabine, with most grade 3 or higher events resulting from myelosuppression. Given the advanced age of the patient cohort, only three individuals (9%) proceeded to transplantation. Cox regression analysis identified post-treatment RBC TI as the sole factor associated with survival. However, the sensitivity of these analyses was limited by the number of pts.
Oral DEC/CED offers clinical benefits for CMML pts and has a generally well-tolerated safety profile. TI could be linked to extended survival.
Source: https://clml-soho2023.elsevierdigitaledition.com/374/index.html
Clinical Trials: https://classic.clinicaltrials.gov/ct2/show/NCT02103478
https://classic.clinicaltrials.gov/ct2/show/NCT03306264
Savona, M.R., McCloskey, J.K., Griffiths, E.A., Yee, K.W.L., Zeidan, A.M., Al-Kali, A., Deeg, H.J., Patel, P.A., Sabloff, M., Keating, M-M., Zhu, N., Gabrail, N., Fazal, S., Maly, J., Odenike, O., Kantarjian, H.M., DeZern, A.E., O’Connell, C.L., Roboz, G.J., Busque, L., Buckstein, R., Amin, H., Randhawa, J.K., Leber, B., Dao, K-H., Sano, Y., Mirakhur, B., Chan, W., Oganesian, A., Keer, H., Garcia-Manero, G. Efficacy and Safety of Oral Decitabine/ Cedazuridine (ASTX727) in the CMML Subpopulation from Phase 2 and ASCERTAIN Phase 3 Studies.