KEY TAKEAWAYS
- The phase 2 ImmunoADAPT trial aimed to study the impact of combining immunotherapy (avelumab) with endocrine therapy ± CDK4/6 inhibitor in ER+ breast cancer.
- The primary endpoint wasn’t met due to low cCR/pCR rates in the palbo arm. Palbo+ET showed increased response after avelumab, suggesting synergy.
- More research is required to explore TME impact on PD-L1 responses. Future studies in high-risk patients are needed.
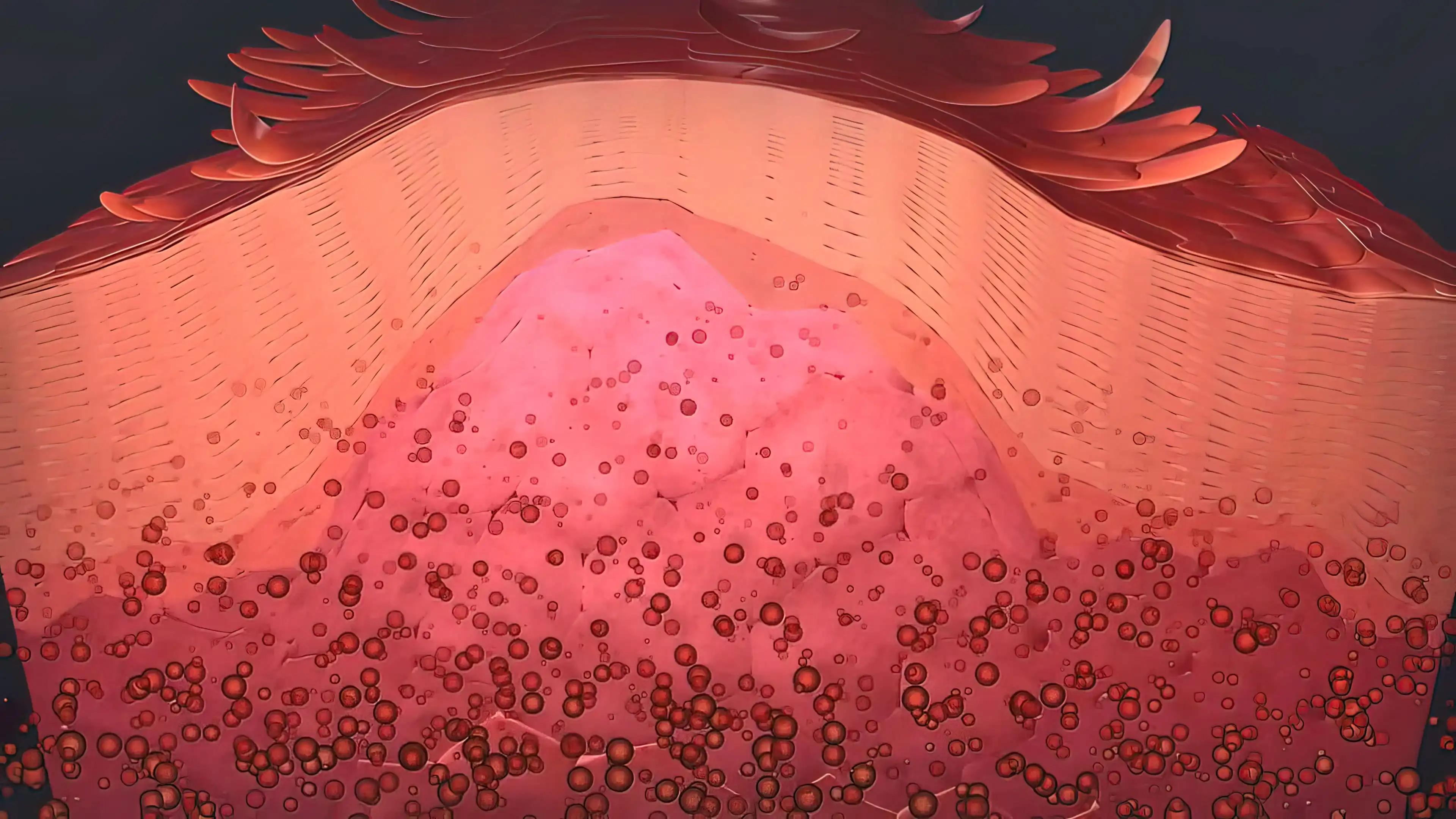
Preclinical and clinical evidence indicates that CDK4/6 inhibitors may enhance the tumor microenvironment’s response to immune factors. This randomized phase 2 pilot study aimed to investigate the impact of CDK4/6 inhibition in combination with immunotherapy in patients with stage II/III ER-positive breast cancer.
P. Zavras and his research team evaluated neoadjuvant endocrine therapy with a PD-L1 inhibitor (avelumab) alone and in combination with a CDK4/6 inhibitor (palbociclib, palbo) to understand their varied effects.
Patients with stage II/III ER+, HER2-negative breast cancer were assigned to different treatment arms. It involved endocrine therapy combined with avelumab, either with or without palbociclib (palbo). Avelumab was administered following a lead-in of endocrine therapy with or without palbociclib for one month, continuing for three more cycles before surgery.
Patients underwent tumor assessments via breast MRIs, evaluated by RECIST 1.1 criteria at multiple points. The primary goal was to observe clinical complete response (cCR) by MRI in the palbociclib arm, with secondary measures including pathologic complete response (pCR), overall response rates (ORR), changes in tumor size, and adverse effects. Researchers also examined additional translational data such as imaging mass cytometry and biomarkers.
Between 2018 and 2023, they enrolled 33 participants, with 30 deemed eligible for primary analysis. Among them, 20 patients received treatment involving palbociclib (palbo), while 10 were in the control group. The demographic and disease-related characteristics were generally well-matched between the two groups, except for a higher prevalence of patients with node-positive disease in the palbociclib group (80% vs. 60%).
The study’s primary objective wasn’t met, as only one patient achieved complete clinical and pathologic responses in the palbociclib group (cCR/pCR rate 4.8%), while no patients in the control group achieved this response. Although the response rates appeared higher in the palbociclib group (42.9% vs. 11.1%), the difference did not reach statistical significance.
Researchers also observed changes in tumor size: after one month of endocrine therapy (ET) combined with palbociclib, the mean tumor size decreased by 11.6%, compared to a 9.4% decrease in the ET-only control group. When avelumab was added to both treatment arms, the mean tumor size decreased by an additional 15.2% in the palbociclib group but increased by 6.9% in the control group (p=0.018).
They conducted a subgroup analysis within the palbociclib arm and found no specific clinical or pathological variables significantly associated with treatment responses. Additionally, they noted a few severe immune-related adverse events, such as autoimmune diabetes, hepatitis, and colitis. Although these were expected due to the nature of the treatment, they were relatively rare.
Previous studies indicated that the addition of palbociclib (palbo) to endocrine therapy (ET) did not notably enhance responses in the neoadjuvant setting. However, when palbociclib was combined with a PD-L1 inhibitor (avelumab), increased responses were observed compared to ET alone. This suggests a potential synergy between endocrine therapy, palbociclib, and avelumab.
The potential of such synergistic effects observed in the study warrants deeper investigation into the underlying changes within the tumor microenvironment. These efforts, through translational analysis, aim to decode the intricate dynamics that enhance responses to PD-L1 inhibitors. The findings suggest future research initiatives are necessary, particularly in high-risk patient groups. These studies should evaluate the acceptability of immunotherapy’s side effects in these cohorts.
The study is sponsored by the Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins.
Source: https://atgproductions.net/atgclients/sabcs/2023_SABCS_Abstract_Report-12-1-23_Compressed.pdf
Clinical Trial: https://clinicaltrials.gov/study/NCT03573648
Zavras P., Chen R., Qi H., et al. (2023). “Neoadjuvant endocrine therapy and avelumab with or without palbociclib in stage II/III endocrine receptor-positive breast cancer: the ImmunoADAPT trial.” Presented at the SABCS 2023 – 46th Annual San Antonio Breast Cancer Symposium, December 05 – December 09, 2023, San Antonio, TX, US (Abstract PO1-01-09).