KEY TAKEAWAYS
- The phase 2 trial aimed to investigate the efficacy and tolerability of zanu, obin, and ven (BOVen) in untreated TP53-mutant MCL.
- The primary endpoint was to determine PFS.
- Researchers noticed promising outcomes with BOVen; further information will be provided later.
TP53-mutant mantle cell lymphoma (MCL) poses a significant challenge with poor survival outcomes under chemoimmunotherapy (Eskelund, Blood 2017), with median progression-free survival (PFS) of 0.9 years and median overall survival (OS) of 1.8 years, lacking a standard frontline treatment. Synergistic activity of Bruton’s tyrosine kinase (BTK) and BCL2 inhibition in relapsed MCL, including TP53 mutation cases, offers a promising avenue (Tam, NEJM 2018). Obinutuzumab (Obin), ibrutinib, and venetoclax (ven), show efficacy in relapsed and untreated MCL (Le Gouill, Blood 2021).
Anita Kumar and her team aimed to assess the hypothesis that zanubrutinib (Zanu), Obin, and Ven in combination (BOVen) could be well-tolerated and efficacious in untreated TP53-mutant MCL
The study performed an inclusive analysis within a multicenter, investigator-initiated phase 2 trial (NCT03824483), enrolling patients (pts) with previously untreated MCL characterized by TP53 mutation (of any variant allele frequency) and an Eastern Cooperative Oncology Group performance status (ECOG PS) of ≤2. Eligibility criteria included an absolute neutrophil count (ANC) >1, platelet count (PLT) >75, and hemoglobin (HGB) ≥9, (unless if due to MCL). The administered treatment, BOVen, followed a 28-day cycle with Zanu at 160 mg orally twice daily from Day 1, Obin at 1000 mg intravenously on Day 1 or split over Days 1-2, 8, 15 of Cycle 1 and Day 1 of Cycles 2-8, and Ven with a ramp-up initiated on C3D1 (target 400 mg QD).
The specified treatment duration was a minimum of 2 years, and the primary endpoint of the study was the 2-year PFS. Response evaluation utilized Lugano criteria (Cheson, JCO 2014), and PFS and OS were estimated using the Kaplan-Meier method. Peripheral blood minimal residual disease (PB-MRD) assessment employed the Adaptive clonoSEQ® assay, allowing discontinuation of Zanu and Ven after 24 cycles if undetectable MRD (<10-6) complete remission (CR) was achieved. Subsequent PB-MRD monitoring facilitated retreatment decisions based on clinical or MRD detectability (>10-6). Adverse events (AE) were assessed according to CTCAE v5.
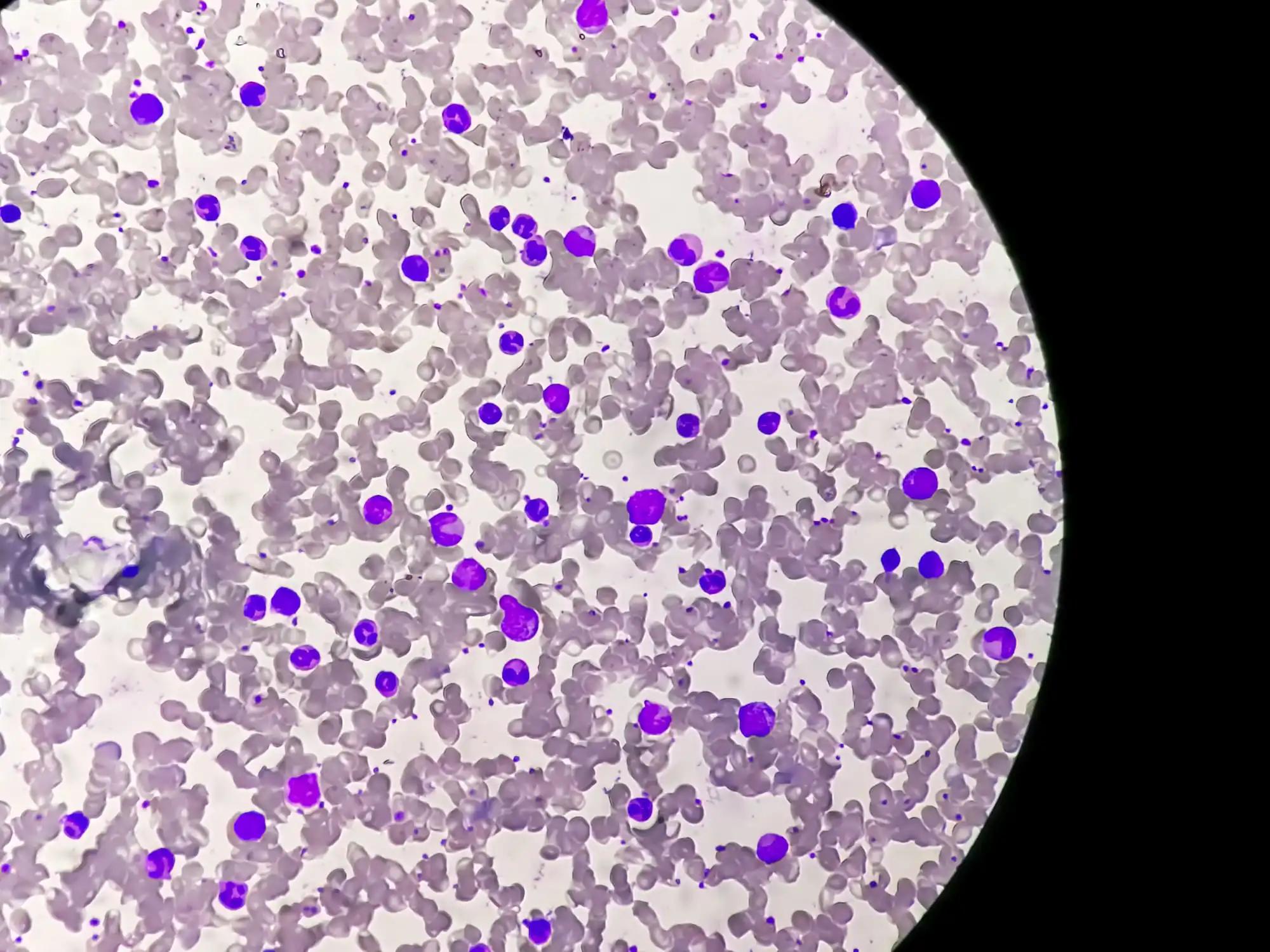
About 25 pts with previously untreated TP53-mutant MCL were enrolled in the study (data cut on May 15, 2023). The median age was 65 years (range 29 – 82), with 76% male (19/25) and various histologic subtypes represented (15 conventional MCL, 5 non-nodal leukemic, and 5 blastoid variants). All pts were at stage IV (100%, 25/25), with MIPI scores categorized as 68% high risk (17/25), 28% intermediate risk (7/25), and 4% low risk (1/25). A significant portion had Ki67 ≥30% (67%, 14/21) and Ki67≥50% (33%, 7/21). All pts had TP53 mutation, and 48% had 17p deletion (12/25).
The treatment was generally well-tolerated, with common treatment-related (TRAEs) being predominantly low-grade and manageable. These included diarrhea (52%), neutropenia (28%), infusion-related reaction (24%), bruising (20%), COVID-19 infection (20%), nausea (20%), thrombocytopenia (20%), and rash (20%). Grade 3 or higher treatment-related AEs occurred for neutropenia (12%), infusion-related reaction (8%), COVID-19 (8%), diarrhea (4%), transaminitis (4%), thrombocytopenia without bleeding (4%), and rash (4%). Detailed toxicity data will be presented in the future.
The median follow-up was 16.1 months, during which there were 5 progressions and 4 deaths on study (2 COVID-related, 1 post-operative aspiration pneumonia, 1 unknown cause). Notably, all deaths occurred in pts who were in ongoing response at the time of death. The best overall response rate was 95% (24/25) with 88% (22/25) achieving a CR. At Cycle 3 post Zanu-Obin, 68% (n=17/25) achieved PET-CR, and post cycle 3, 5 pts converted to a PET-CR. The 1-year PFS and OS were 84% (95% CI: 71%, 100%) and 96% (95% CI: 89%, 100), respectively. The 16-month PFS and OS were 75% (95% CI: 60%, 95%) and 87% (95% CI: 75%, 100%), respectively. Specifically for pts less than 65 years of age (n=9), both the 16-month PFS and OS were 100%. About 7 pts completed 24 treatment cycles, of which 71% (5/7 pts) achieved CR and MRD undetectable (treatment discontinued), and 29% (2/7 pts) were in CR and MRD detectable (continued treatment). Outcomes post Cycle 24 will be presented in the future. At the 10-6 MRD sensitivity level, 7 (28%) of 23 pts had undetectable MRD at Cycle 3, and 16 (100%) of 16 pts at Cycle 13.
The study concludes that BOVen is a well-tolerated outpatient regimen showing high response rates and substantial rates of undetectable MRD in untreated TP53-mutant MCL. Early PFS and OS estimates compare favorably with historical chemoimmunotherapy outcomes, establishing BOVen as a promising treatment option for TP53-mutant MCL. The study’s success led to an expansion, including an additional 25 (total 50) TP53-mutant MCL pts. The trial is ongoing, and results are yet to be presented.
The study is sponsored by Memorial Sloan Kettering Cancer Center
Source: https://ash.confex.com/ash/2023/webprogram/Paper180069.html
Clinical Trial: https://clinicaltrials.gov/study/NCT03824483
Kumar A, Soumerai J, Abramson J S, et al. (2023). “A Multicenter Phase 2 Trial of Zanubrutinib, Obinutuzumab, and Venetoclax (BOVen) in Patients with Treatment-Naïve, TP53-Mutant Mantle Cell Lymphoma.” Presented at ASH 2023 (Abstract 738).