KEY TAKEAWAYS
- The NEOPEMBROV phase II trial aimed to investigate the efficacy and identify resistance mechanisms of pembro and NACT combination in OC patients.
- Pembro with chemo showed promise for a subset of OC patients, targeting VEGFR2+ cells offered a potential avenue to overcome resistance and benefit a wider population, warranting VEGFR2 inhibitor clinical trials.
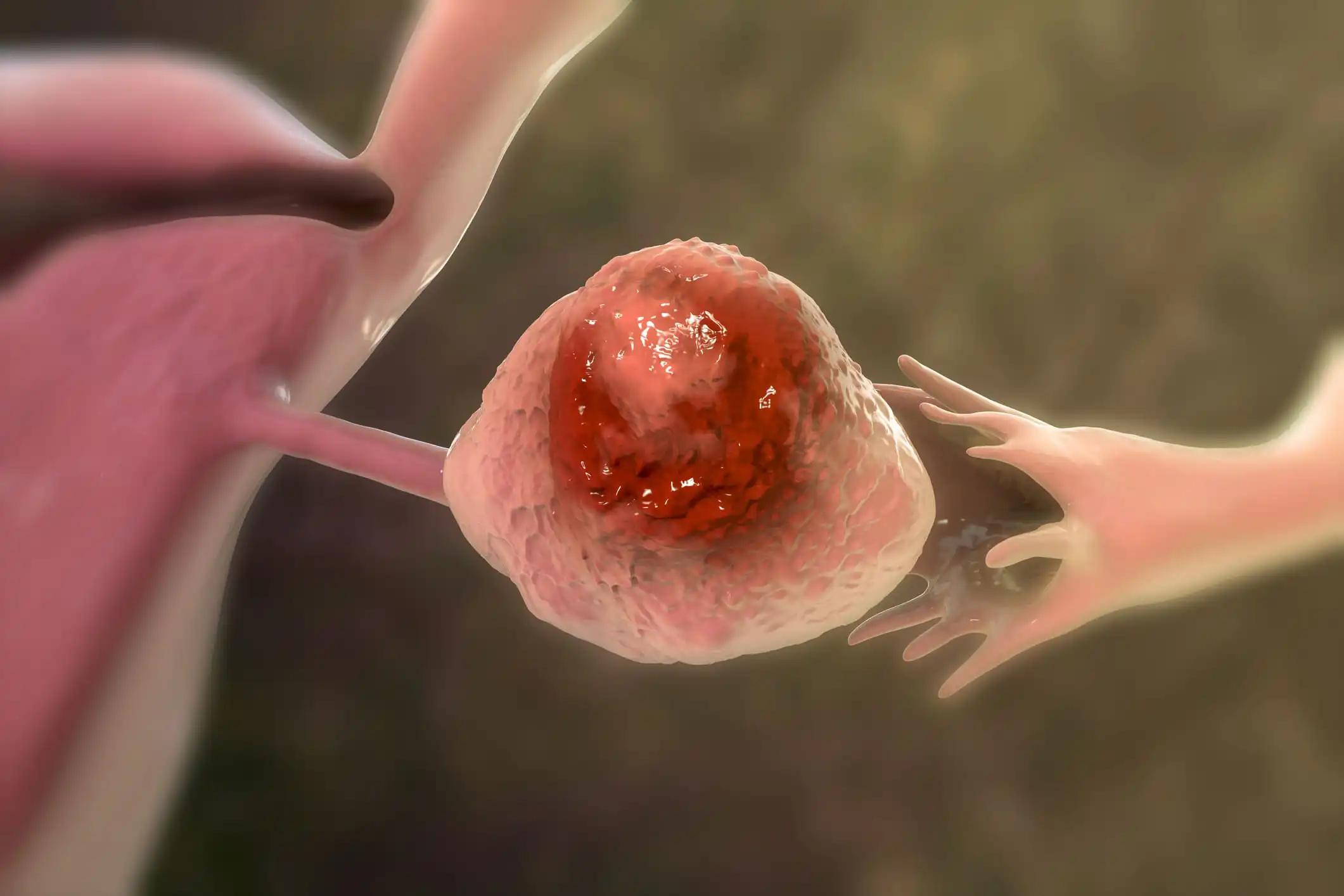
High-grade serous ovarian carcinomas (HGSC) exhibit limited efficacy with immune checkpoint inhibitors (ICI).
Olivia Le Saux and her research team conducted the study that aimed to assess the efficacy and identify resistance mechanisms in the NeoPembrOv randomized phase II trial, evaluating the combination of pembrolizumab (pembro) with neoAdjuvant chemotherapy (NACT).
About 91 patients were randomized in a 2:1 ratio to receive NACT+pembro or NACT alone. Paired samples from 53 patients were subjected to RNA-seq analysis, while multiplexed immunofluorescence staining for CD8, PD-1, ActCasp3, panCK, CD31, and VEGFR2 was performed on samples from 64 patients. Immune and endothelial signatures were evaluated using MCP-counter and quanTIseq algorithms. Cell densities and nearest neighbors were determined through InForm software.
The impact of NACT±P on the tumor microenvironment (TME) and parameters associated with survival were investigated. In the absence of a transcriptomic dataset for high-grade serous carcinomas (HGSC) patients under ICI, an external validation cohort of 102 head and neck cancer patients were utilized.
The analysis of differentially expressed genes (DEG) revealed a notable enrichment of T cell activation/differentiation pathways exclusively in the NACT+P arm post-treatment. A significant rise in CD8+PD-1+ T cell density within tumor islets was demonstrated in the NACT+P arm compared to NACT alone (p=0.015). This observed increase, seen in 15% of cases (n=6/41), correlated with improved overall survival (OS) (LR test, P=0.01). Following NACT+P, the median distance between apoptotic tumors and the nearest CD8+PD-1+ cell significantly decreased.
Univariate Cox models identified a negative association between the MCP-counter endothelial cell signature and survival (HR=1.97, 95% CI [1.10-3.49], P=0.02) in the NACT+P arm, with a significant interaction with the treatment arm (P=0.046). In situ analysis confirmed the negative predictive impact of high VEGFR2 expression on CD31+ endothelial cells in NACT+P-treated patients, significantly affecting OS (P=0.005). KDR expression (VEGFR2) was validated as a predictive biomarker for OS in an external cohort (P=0.044).
The results showed that the efficacy of ICI is limited in a subset of HGSC patients. Combining pembro, along with targeting VEGFR2+ endothelial cells, emerges as a potential strategy to overcome resistance. There is a pressing need for clinical trials to evaluate the efficacy of VEGFR2 inhibitors in this context. Research is sponsored by ARCAGY/ GINECO GROUP.
Source: https://cslide.ctimeetingtech.com/immuno23hybrid/attendee/confcal/show/session/34
Clinical Trial: https://clinicaltrials.gov/study/NCT03275506
Le Saux O et al. (2023) ‘’Immunogenomic profiling of the randomized NeoPembrOv clinical trial reveals the VEGFR2 angiogenic axis as a promising actionable target to overcome immunoresistance of high-grade ovarian carcinomas.’’ Presented at ESMO I-O 2023 (180P).