KEY TAKEAWAYS
- The BRUIN phase 1/2 trial aimed to investigate the safety and efficacy of pirtobrutinib monotherapy in patients with Richter transformation.
- The primary endpoint was to determine ORR.
- Researchers observed that pirtobrutinib shows promising safety and efficacy in Richter transformation, suggesting further exploration is needed.
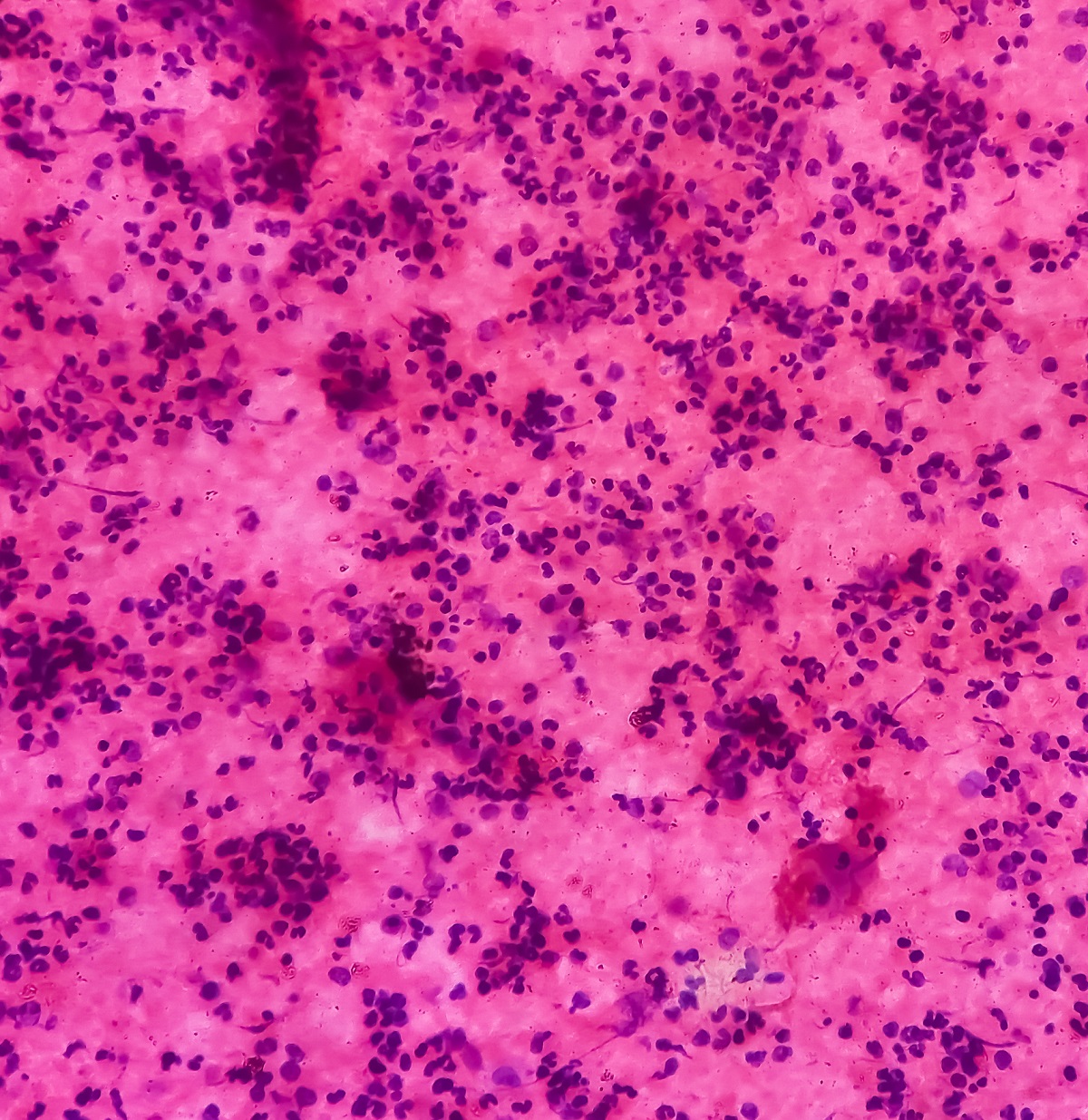
Richter transformation, an aggressive form of diffuse large B-cell lymphoma (DLBCL), occurs in up to 10% of patients with chronic lymphocytic leukemia (CLL) and is associated with a poor prognosis and no approved therapies.
Pirtobrutinib, a selective and reversible Bruton tyrosine kinase (BTK) inhibitor, has demonstrated promising efficacy and tolerability in patients with relapsed or refractory (R/R) B-cell malignancies, including those who have progressed on covalent BTK inhibitors.
William G. Wierda and the team aimed to evaluate the safety and effectiveness of pirtobrutinib monotherapy in a subgroup of patients with Richter transformation from the multicenter, open-label, phase 1/2 BRUIN study.
They performed an inclusive analysis involving adult patients (aged ≥18 years) with histologically confirmed Richter transformation, an Eastern Cooperative Oncology Group performance status score of 0-2, and no limit on previous therapies, including those receiving first-line (1L) treatment per a protocol amendment (version 9.0, Dec 15, 2021). Pirtobrutinib 200 mg was administered orally once daily in 28-day cycles.
The primary endpoint of phase 1 of the BRUIN trial, previously reported, was to establish the recommended phase 2 dose for pirtobrutinib monotherapy, while the primary endpoint of phase 2 was the overall response rate (ORR). Safety and activity were assessed in all patients who received at least 1 dose of pirtobrutinib monotherapy.
About 82 patients were enrolled between Dec 26, 2019, and July 22, 2022, with 5 patients enrolled during phase 1 and 77 during phase 2. However 1 patient received a starting dose of 200 mg pirtobrutinib once daily as the recommended phase 2 dose; the remaining patient received 150 mg pirtobrutinib once daily, which was not escalated to 200 mg.
The median age of patients was 67 years (IQR 59-72). Of the 82 patients, 55 (67%) were male and 27 (33%) were female. Most patients were White (65 [79%] of 82). A total of 74 (90%) of 82 patients had received at least 1 previous Richter transformation-directed therapy, with 61 (74% of 82) having received prior covalent BTK inhibitor therapy for chronic lymphocytic leukemia or Richter transformation.
The ORR was 50.0% (95% CI 38.7-61.3). In which 11 (13%) of 82 patients achieved a complete response, and 30 (37%) of 82 patients had a partial response. Of these 8 patients with ongoing responses elected to discontinue pirtobrutinib to undergo stem-cell transplantation. The most common grade 3 or worse adverse event (AE) was neutropenia (n=19). There were no treatment-related deaths.
The study concluded that pirtobrutinib demonstrates promising safety and activity in patients with Richter transformation, including those who had previously received Richter transformation-directed therapy and covalent BTK inhibitors.
These findings support further investigation of pirtobrutinib as a potential treatment option for patients with R/R Richter transformation after prior treatment with covalent BTK inhibitors.
The trial was sponsored by Loxo Oncology, Inc.
Source: https://pubmed.ncbi.nlm.nih.gov/39033770/
Clinical Trial: https://clinicaltrials.gov/study/NCT03740529
Wierda WG, Shah NN, Cheah CY, et al. (2024). “Pirtobrutinib, a highly selective, non-covalent (reversible) BTK inhibitor in patients with B-cell malignancies: analysis of the Richter transformation subgroup from the multicentre, open-label, phase 1/2 BRUIN study.” Lancet Haematol. 2024;11(9):e682-e692. doi:10.1016/S2352-3026(24)00172-8