KEY TAKEAWAYS
- The phase II trial aimed to determine if patients with undetectable post-operative HPV ctDNA could safely undergo active surveillance without immediate adjuvant radiation.
- The study concluded that post-operative HPV ctDNA-based patient selection for active surveillance needs refinement due to high recurrence rates.
In head and neck cancers, Human Papilloma Virus cell-free tumor DNA (HPV ctDNA) might detect residual disease before clinical recurrence manifests.
Linda Chen and the team spearheaded a study that aimed to assess if patients with undetectable post-operative HPV ctDNA could undergo active surveillance, delaying adjuvant radiation until HPV ctDNA detection.
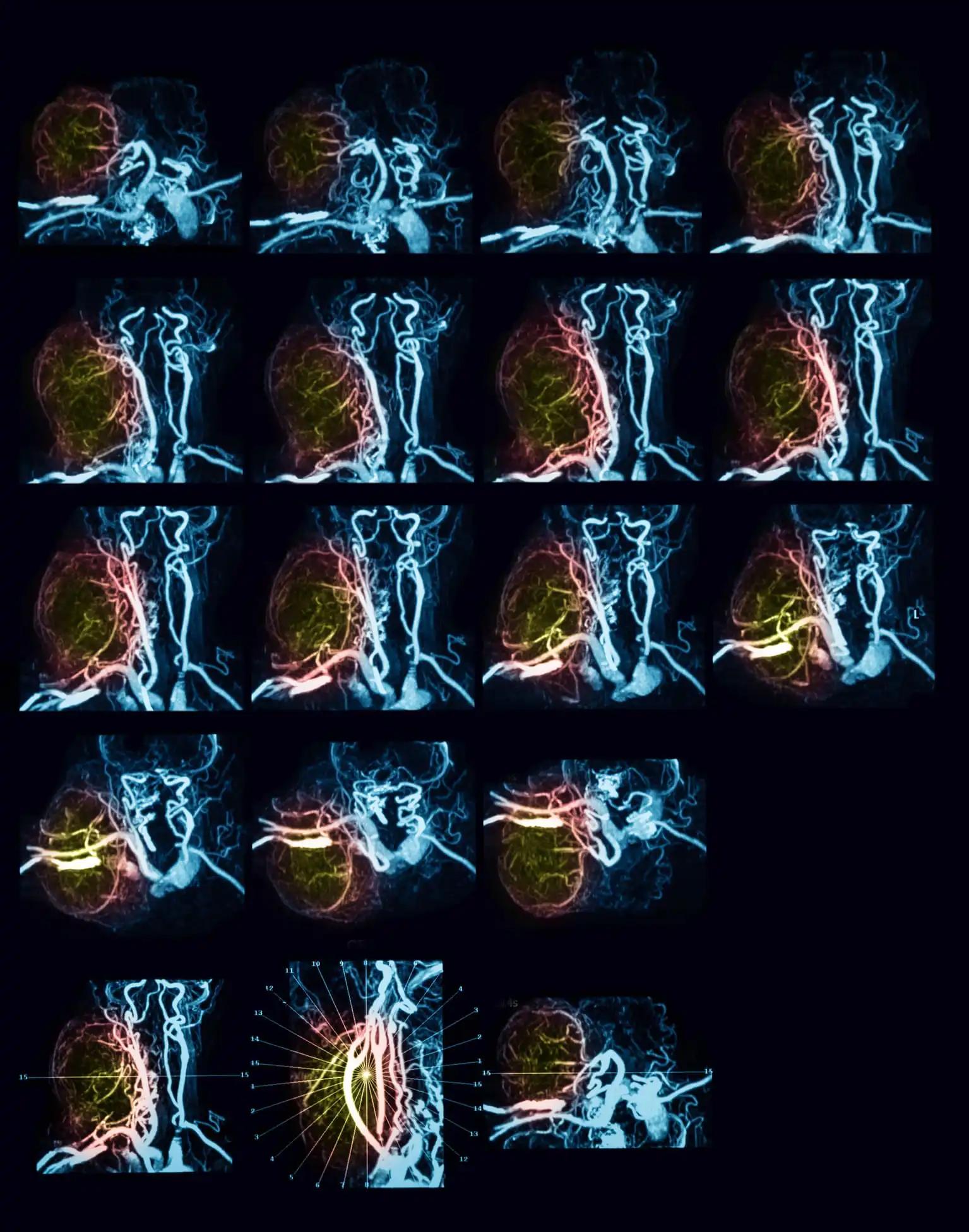
The study evaluated HPV ctDNA using the NavDx assay (Naveris, Inc.), quantifying circulating tumor tissue modified viral (TTMV)-HPV DNA. Eligible subjects had a preoperative TTMV-HPV DNA Score of ≥50 fragments/mL, underwent complete surgical resection of all gross disease as confirmed by post-operative MRI, possessed at least one pathologic risk factor for adjuvant therapy, and tested negative for post-operative HPV ctDNA in two draws 2-6 weeks after surgery.
Throughout active surveillance, patients underwent TTMV-HPV DNA testing, imaging, and examination every 3 months (mo). Patients were considered for delayed adjuvant radiation only if they developed detectable TTMV-HPV DNA without evidence of gross disease. The primary endpoint suggested further study if ≥85% of evaluable patients (n=15 in each cohort) remained free of gross disease progression at one year.
Among the 53 patients screened, 12 were enrolled in Cohort A before early closure. Exclusions included TTMV-HPV DNA Score <50 frag/mL (n=21) and positive margin or extracapsular extension (n=11), including 2 patients with a positive post-operative TTMV-HPV DNA score. The median pre-treatment TTMV-HPV DNA Score for enrolled Cohort A patients was 448 (Range: 59-2135 frag/mL), with a median follow-up of 12.5 months (Range: 3.7-21 months).
The study detected TTMV-HPV DNA during surveillance in 1 of the 12 patients, 6 months post-surgery, without gross disease evidence; this patient received 60 Gy of adjuvant radiotherapy. At the 6-month surveillance, 3 additional patients exhibited radiographic disease progression, occurring synchronously (n=2) or preceding TTMV-HPV DNA detection (n=1). Cohort A closed due to 3 of 12 patients developing gross recurrent disease, failing to meet the primary endpoint. Cohort B (de-escalated post-operative therapy) remains open and will be reported separately.
The study concluded that the pilot approach, utilizing HPV ctDNA-based patient selection for post-operative active surveillance, resulted in a notable rate of gross disease recurrence, failing to meet the primary endpoint. Radiographic recurrence occurred without preceding detectable TTMV-HPV DNA during 3-month interval surveillance.
This highlights the need for additional clinical factors to guide patient selection for active surveillance and the timing of delayed adjuvant therapy initiation before recurrence. Research was funded by Memorial Sloan Kettering Cancer Center.
Source: https://astro.confex.com/astro/hncs2024/meetingapp.cgi/Paper/60851
Clinical Trial: https://clinicaltrials.gov/study/NCT05307939
Chen L, Cohen M, Hatzoglou V, et al. (2024) ‘’Early Disease Recurrence Following Post-operative HPV ctDNA Directed Active Surveillance in Oropharyngeal Carcinoma – Outcomes of a Prospective Pilot Study.’’ Presented at MHNCS 2024 (LBA 01).