KEY TAKEAWAYS
- The ANTICIPATE phase I/II trials aimed to explore the efficacy of APL-1202 combined with tislelizumab as NACT in MIBC patients.
- The primary endpoint was pCR.
- The results showed both groups exceeded thresholds for stage 2 expansion. Safety and efficacy support further evaluation of APL-1202 plus tislelizumab.
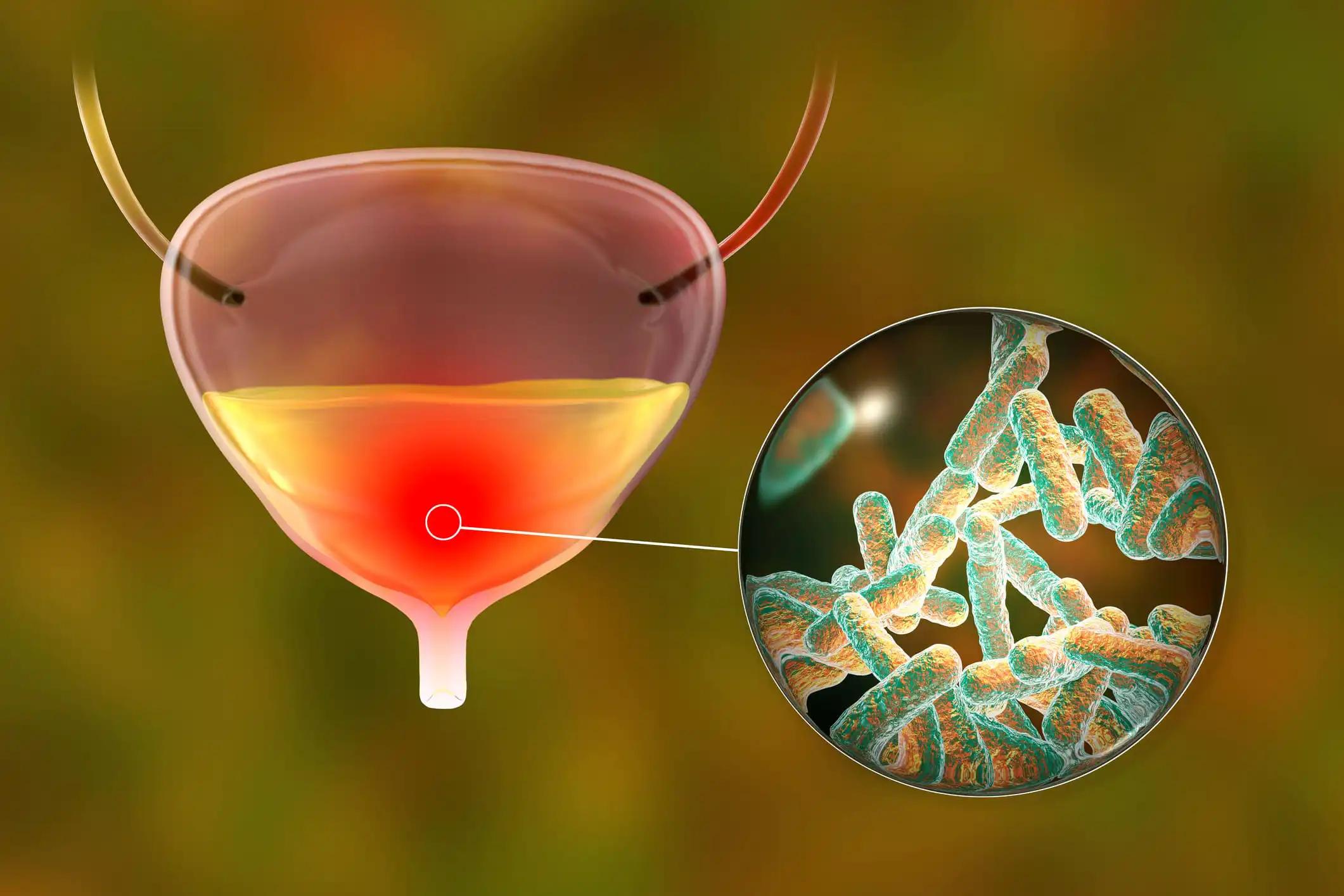
Muscle-invasive bladder cancer (MIBC) often requires aggressive treatment. APL-1202 (nitroxoline), a reversible MetAP2 inhibitor, exhibits anti-angiogenic and anti-tumor properties. While single-agent neoadjuvant programmed death 1 (PD-1) antibodies can achieve pathological complete responses (pCR) in some MIBC patients, combining APL-1202 with PD-1 antibodies has synergistic effects in various cancer models, including bladder cancer.
Matt D. Galsky and his team spearheaded a study by hypothesizing that combining APL-1202 with tislelizumab, a humanized IgG4 anti-PD-1 antibody, could be effective neoadjuvant therapy (NACT) for MIBC.
This prospective multicenter randomized phase II trial targeted newly diagnosed MIBC patients slated for radical cystectomy (RC) but were ineligible for cisplatin or decline cisplatin-based NACT. Participants were randomly allocated to either group 1 (APL-1202 plus tislelizumab) or group 2 (tislelizumab), with randomization stratified by PD-L1 expression.
The NACT was administered every 3 weeks for 3 cycles. The primary endpoint was the pathological complete response (pCR, pT0N0) rate. Employing Simon’s 2-stage design, planned interim analyses occurred after 18 evaluable patients in group 1 and 14 evaluable patients in group 2.
About 42 patients were enrolled, with results available for 32 evaluable patients in stage 1 of the 2-stage design. Radical cystectomy was completed in all 18 patients in group 1 and 13 out of 14 patients in group 2. Only 1 patient could not undergo surgery due to disease progression, and 10 patients refused radical cystectomy.
Among the 32 evaluable patients, 11 out of 18 (61%) and 10 out of 14 (72%) had cT2 tumors in groups 1 and 2, respectively. Additionally, 6 out of 18 (33%) and 2 out of 14 (14%) had cT3 tumors, and 1 out of 18 (6%) and 2 out of 14 (14%) had cT4a tumors in groups 1 and 2, respectively. PD-L1 expression was evaluated using the VENTANA PD-L1 (SP263) Assay, with 8 out of 18 (44%) patients in group 1 and 7 out of 14 (50%) in group 2 testing positive.
Treatment-emergent adverse events (TEAEs) were observed in 17 (94.4%) patients in group 1 and 11 (78.6%) in group 2. The most common (≥ 10%) TEAEs of CTCAE grade ≥ 3 were anemia (4, 22.2%) and decreased lymphocyte count (3, 16.7%) in group 1 and intestinal obstruction (3, 21.4%) in group 2. AEs led to drug discontinuation in 3 (16.7%) patients in group 1 (acute kidney injury, anemia, hepatic function abnormal) and 2 (14.3%) in group 2 (immune hyperthyroidism, COVID-19), with no TEAEs resulting in death.
The study concluded that group 1 (APL-1202 plus tislelizumab) and group 2 (tislelizumab) surpassed the thresholds for stage 2 expansion in the 2-stage design. The observed activity and safety of neoadjuvant APL-1202 plus tislelizumab warrant continued evaluation of this innovative regimen. Research was funded by Jiangsu Yahong Meditech Co., Ltd aka Asieris.
Source: https://meetings.asco.org/abstracts-presentations/230645
Clinical Trial: https://clinicaltrials.gov/study/NCT04813107
Galsky MD, Sfakianos JP, Ye D, et al. (2024) ‘’Oral APL-1202 in combination with tislelizumab as neoadjuvant therapy in patients with muscle-invasive bladder cancer (MIBC): Interim analysis of ANTICIPATE phase II trial.’’ J Clin Oncol 42, 2024 (suppl 4; abstr 632). DOI: 10.1200/JCO.2024.42.4_suppl.632