KEY TAKEAWAYS
- The study aimed to investigate PD-L1 in PTC, assessing its prognostic significance and correlation with clinicopathological variables and addressing a critical gap in understanding thyroid cancer.
- Researchers observed a significant interplay between CLLT, oncocytic metaplasia, and PD-L1 expression in PTC; further investigation is ongoing.
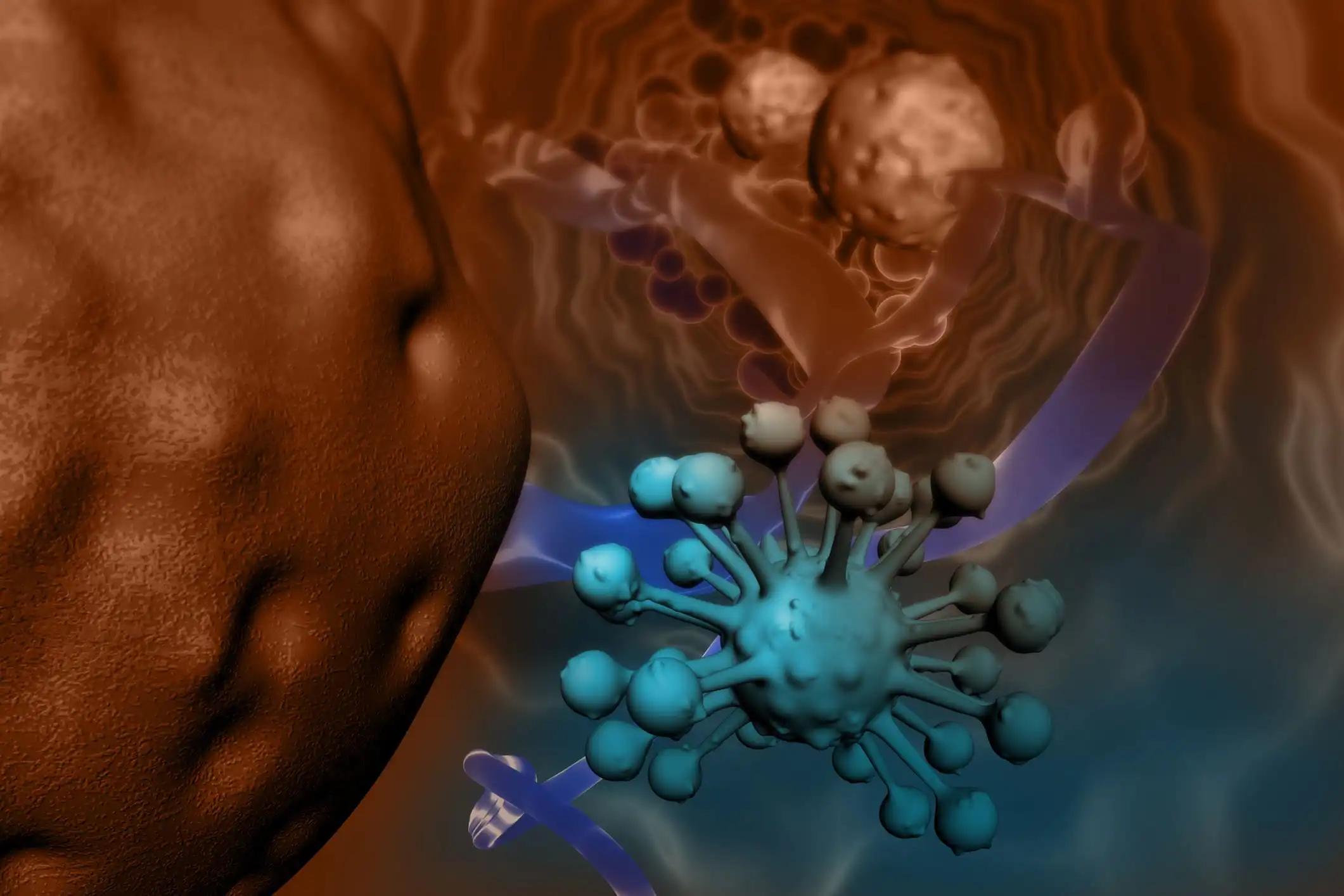
Despite PD-L1’s established role in predicting immunotherapeutic responses in malignancies, its significance and prognostic implications in papillary thyroid cancer (PTC) are insufficiently explored.
Vitor Barreto Santana and the team aimed to bridge this gap by thoroughly analyzing PD-L1 expression in PTC and examining its correlation with key clinicopathological variables.
Researchers performed an inclusive analysis employing immunohistochemistry (IHC) to evaluate PD-L1 expression in whole-tissue sections from 121 primary PTC cases. The investigation meticulously examined correlations between PD-L1 expression and diverse clinicopathological variables to elucidate the nuanced associations within the study cohort.
About 33.1% of PTCs displayed PD-L1 expression, primarily manifesting weak to moderate intensity. Notably, no significant correlation emerged between PD-L1 expression and clinicopathological variables, including age, sex, histological subtype, and tumor size. This observation underscores the intricate and multifaceted regulation of PD-L1 in PTC.
In multivariate logistic regression analysis, chronic lymphocytic thyroiditis with oncocytic metaplasia emerged as the exclusive independent predictor of PD-L1 expression (P = 0.014), emphasizing the potential impact of the tumor microenvironment (TME) on immune checkpoint expression in PTC.
The study concluded that the intricate interplay between chronic lymphocytic thyroiditis with oncocytic metaplasia and PD-L1 expression in PTC suggests a potential therapeutic avenue with anti-PD-1/PD-L1 therapies for surgery-refractory cases. Understanding the dynamics of immune checkpoint regulation within the tumor microenvironment is crucial for effective treatment strategies.
Future research should explore the molecular mechanisms underlying this interaction and its implications for patient outcomes, contributing valuable insights to the evolving field of thyroid cancer immunotherapy. The study received no funds.
Source: https://pubmed.ncbi.nlm.nih.gov/38457034/
Santana VB, Krüger VM, Abrahão MCY, et al. (2024). ‘’Chronic Lymphocytic Thyroiditis with Oncocytic Metaplasia Influences PD-L1 Expression in Papillary Thyroid Carcinoma.’’ Head Neck Pathol. 2024 Mar 8;18(1):14. doi: 10.1007/s12105-024-01618-5. PMID: 38457034; PMCID: PMC10923758.