KEY TAKEAWAYS
- The study aimed to investigate combining CB-HCT with AML-specific TCR-engineered T-cell therapy for pediatric AML.
- Researchers noticed the feasibility of potent CB-derived CD8+ T cells targeting WT1, which shows promise for preventing relapse in patients with pediatric AML.
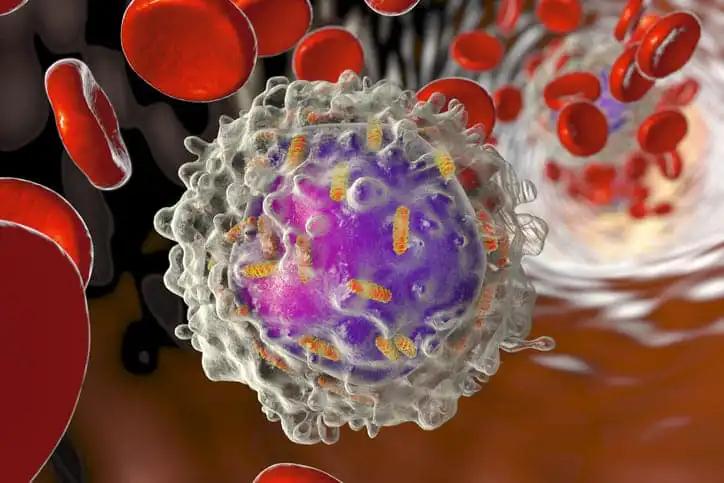
Hematopoietic cell transplantation (HCT) is an effective treatment for pediatric patients facing high-risk, refractory, or relapsed acute myeloid leukemia (AML). Despite its effectiveness, a significant proportion of transplanted individuals succumb to relapse, necessitating novel therapeutic approaches to enhance overall survival rates.
Vania Lo Presti and her team aimed to propose a synergistic strategy combining cord blood (CB)-HCT with AML-specific T cell receptor (TCR)–engineered T cell therapy derived from the same CB graft.
Researchers performed an inclusive analysis, generating CB-CD8+ T cells expressing a recombinant TCR (rTCR) targeting Wilms tumor 1 (WT1) while devoid of endogenous TCR (eTCR) expression to prevent mispairing and competition. CRISPR-Cas9 multiplexing targeted the constant region of endogenous TCRα (TRAC) and TCRβ (TRBC) chains.
Subsequently, an optimized lentiviral transduction method introduced recombinant WT1-TCR. Evaluation encompassed cytotoxic and migratory capabilities through coculture assays involving cell lines and primary pediatric AML blasts.
The gene editing and transduction procedures achieved high efficiency, resulting in up to 95% of cells lacking eTCR and over 70% of T cells expressing rWT1-TCR. WT1-TCR-engineered T cells lacking the expression of their eTCR (eTCR-/- WT1-TCR) exhibited increased cell surface expression of the rTCR and produced cytotoxic cytokines, including granzyme A and B, perforin, interferon-γ (IFNγ), and tumor necrosis factor-α (TNFα), upon antigen recognition compared to eTCR+/+ WT1-TCR-engineered T cells.
CRISPR-Cas9 editing did not alter immunophenotypic characteristics, T cell activation, or increase inhibitory molecule expression. In coculture experiments, eTCR-/- WT1-TCR CD8+ CB-T cells demonstrated effective migratory and killing capacity against neoplastic cell lines and primary AML blasts while sparing healthy cells from toxicity.
The study concluded by demonstrating the feasibility of developing a potent CB-derived CD8+ T cell product targeting WT1. This innovative approach offers a promising option for post-transplant allogeneic immune cell therapy or as an off-the-shelf product, aiming to prevent relapse and enhance the clinical outcome of children with AML.
The study was sponsored by the Dutch Cancer Society.
Source: https://pubmed.ncbi.nlm.nih.gov/38580329/
Lo Presti V, Meringa A, Dunnebach E, et al. (2024). “Combining CRISPR-Cas9 and TCR exchange to generate a safe and efficient cord blood-derived T cell product for pediatric relapsed AML.” J Immunother Cancer. 2024 Apr 5;12(4):e008174. doi: 10.1136/jitc-2023-008174. PMID: 38580329; PMCID: PMC11002379.