KEY TAKEAWAYS
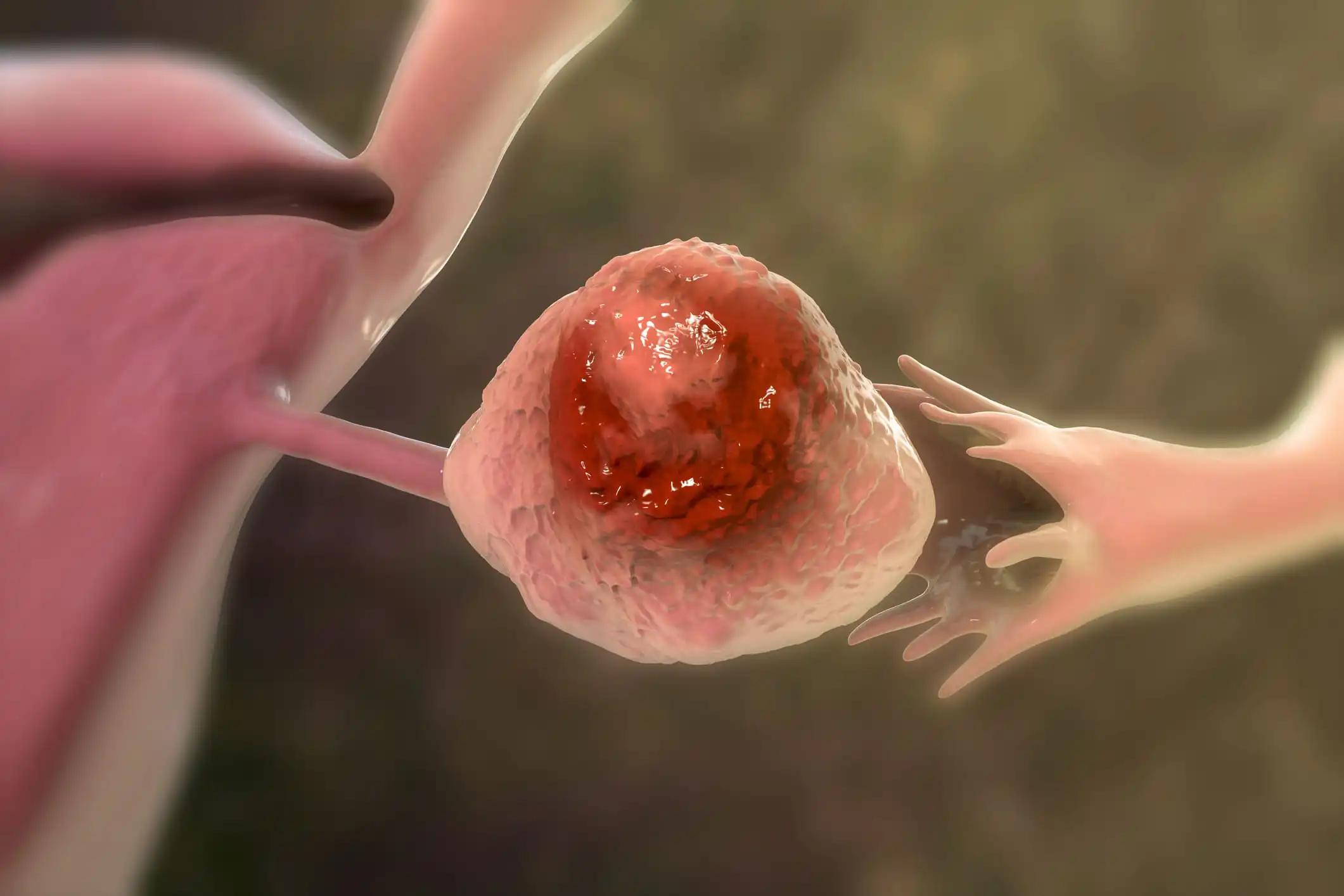
- The phase 1 trial aimed to investigate the enhanced in vivo anti-tumor activity of a fully humanized CAR T targeting mesothelin compared to a murine-derived counterpart, focusing on improving persistence and efficacy.
- Researchers noticed enhanced M5 CAR T cell persistence in mesothelin-expressing cancers, suggesting avenues for improving clinical outcomes in CAR T cell therapy trials.
In the prior study, a CAR T using a murine-derived CAR construct targeted to mesothelin (SS1 CAR) demonstrated limited persistence and efficacy in ovarian cancer (OC).
Janos L. Tanyi and the team aimed to develop a fully human anti-mesothelin scFv fused to 4-1BB (CD137) and CD3zeta (M5 CAR). Pre-clinical evaluation revealed superior in vivo anti-tumor activity compared to SS1 CAR.
They performed an inclusive analysis to determine the maximum tolerated dose (MTD) of 3 x 107 CAR T-meso cells/m2. 19 patients with mesothelin-expressing tumors (14 ovarian, 1 lung, 4 malignant mesothelioma) were treated with the M5 CAR at this dose. 3 patients received a single IV dose of 3 x 107 CAR Ts without lymphodepletion (Cohort 1), 3 patients received a single IV dose of 3 x 107 CAR Ts following lymphodepletion (Cohort 2), and 2 patients received a single intrapleural CAR T infusion of 3 x 107 CAR Ts (cohort 3).
In repeated dose cohorts, 6 patients received an initial IV dose of 3 x 107 CAR T-meso cells/m^2 after lymphodepletion (Cohort 4), and another 5 patients received an intraperitoneal instillation of the same dose (Cohort 5), with all patients receiving up to two additional IV doses spaced 21-42 days apart.
About the treatment outcomes, M5 CAR T cells were detectable in the blood within 1 hour after infusion, peaking at Days 7-10, with higher levels observed in patients after lymphodepletion. Detectable M5 CAR T cells persisted in the blood for up to 28-42 days in all subjects, in 5 patients at 6 months, and in 4 patients at 18 months. M5 CAR T cells trafficked to the tumor in 13 out of 19 patients.
Using RECIST criteria, at 28-35 days after treatment, 13 patients showed stable disease (13/19, 68%) with a maximal target tumor volume decrease of 29.1%. A stable disease for 3 months in 4 patients was seen, and another had a stable disease for 21 months. Cytokine release syndrome (CRS) (1 Grade 3 and 3 Grade 4) was experienced by 9 subjects.
About 4 patients experienced Grade 4 serious adverse events (SAEs) (CRS, hypotension, hypoxia), and 14 patients had grade 3 SAEs (febrile neutropenia, abdominal pain, fatigue, CRS, hyponatremia, dyspnea, hypoxia, hypotension), with all subjects fully recovering.
The study concluded that M5 CAR T cells exhibited engraftment and expansion in the blood of all subjects, with prolonged persistence compared to SS1 CAR, and CAR T trafficking into tumors was identified in 13/19 patients. Despite short-term stable disease in most patients, no RECIST-defined clinical responses were observed. However, CAR T trafficking into tumors was identified in a significant portion of patients, indicating potential efficacy.
Furthermore, all routes of application were deemed safe and well tolerated. These findings suggest avenues for future clinical trials in CAR T cell therapy, particularly exploring combination approaches with oncoviruses, checkpoint inhibitors, or microenvironment modifiers to enhance trafficking, persistence, and clinical response.
The trial was sponsored by the University of Pennsylvania.
Source: https://sgo.planion.com/Web.User/AbstractDet?ACCOUNT=SGO&ABSID=461177&CONF=AM2024&CKEY=
Clinical Trial: https://clinicaltrials.gov/study/NCT03054298
Tanyi J.L., Haas A.R., Aggarwal C, et al. (2024). “Phase I clinical trial of autologous T cells bearing fully humanized chimeric antigen receptors targeting mesothelin with both intravenous administration and local delivery with or without lymphodepletion in mesothelin-expressing cancers, including ovarian cancer.” Presented at SGO 2024 (Abstract 2136).