KEY TAKEAWAYS
- The ATLANTIS trial was a phase 3, open-marker, randomized clinical study to estimate the efficacity and safety of lurbinectedin and doxorubicin combination remedy as an alternate-line treatment for small-cell lung cancer.
- 613 cases were aimlessly assigned to either the lurbinectedin plus doxorubicin or the control group.
- Median overall survival of 8.6 months in the lurbinectedin plus doxorubicin group was observed with a standard follow- up of 24.1 months, compared to 7.6 months in the control group.
- Treatment-related adverse events passed in 88 of the lurbinectedin plus doxorubicin group and 92 of the control group.
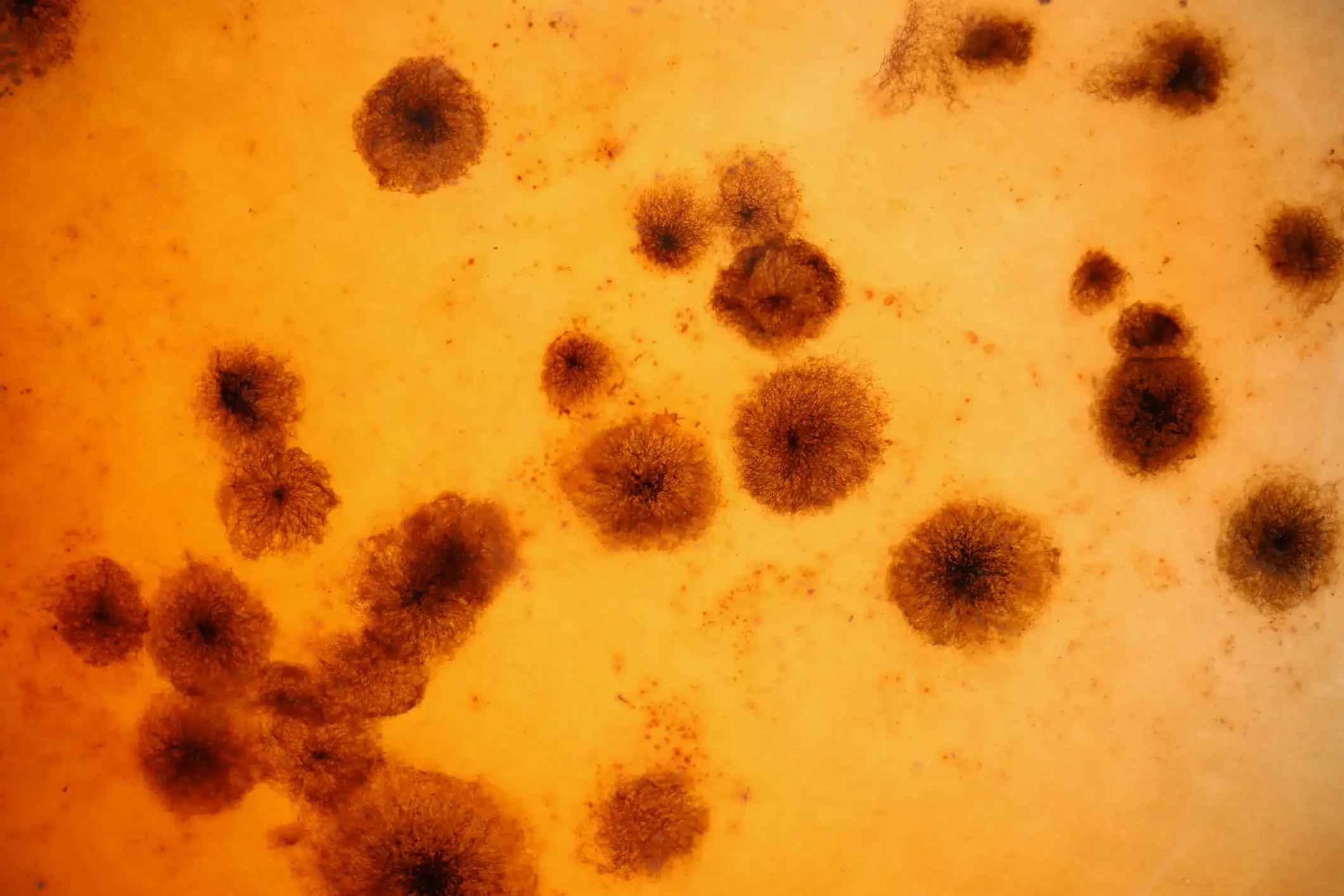
Lurbinectedin is a synthetic marine- a deducedanti-tumor agent that’s a picky asset of oncogenic recap. The US Food and Drug Administration approved lurbinectedin monotherapy(3.2 mg/ m2 every three weeks) grounded on its efficacity in cases with small-cell lung cancer (SCLC) that regressed after first-line platinum-grounded chemotherapy. The ATLANTIS trial estimated the efficacity and safety of the combination of lurbinectedin and anthracycline doxorubicin as an alternate-line treatment for SCLC. This phase 3, open-marker, randomized study included adult cases who progressed 18 times or aged with SCLC and regressed after platinum-grounded chemotherapy.
An aggregate of 613 cases was aimlessly assigned( 11) centrally by dynamic allocation to either an intravenous lurbinectedin2.0 mg/ m2 plus doxorubicin40.0 mg/ m2 administered on day 1 of 21-day cycles or the croaker’s choice of control remedy( intravenous topotecan1.5 mg/ m2 on days 1- 5 of 21- day cycles; or intravenous cyclophosphamide 1000 mg/ m2, doxorubicin45.0 mg/ m2, and vincristine2.0 mg on day 1 of 21- day cycles( CAV)). Primary granulocyte-colony-stimulating factor prophylaxis was obligatory in both treatment groups. Neither cases nor clinicians were apprehensive of treatment allocation, but the independent review commission assessed issues and masked to cases’ treatment allocation.
The primary endpoint was overall survival in the intention-to-treat population. At a standard follow- up of24.1 months, 303 cases in the lurbinectedin plus doxorubicin group and 289 cases in the control group had discontinued study treatment. The most common reason for termination was progressive complaint( 213( 70) cases in the lurbinectedin plus doxorubicin group vs 152( 53) in the control group). The median overall survival was8.6 months( 95 CI7.1-9.4) in the lurbinectedin plus doxorubicin group versus7.6 months(6.6-8.2) in the control group( stratified log- rank p = 0.90; hazard rate0.97( 95 CI0.82-1.15), p = 0.70). Treatment-related adverse events passed in 268( 88) cases in the lurbinectedin plus doxorubicin group and 266( 92) cases in the control group.
Grade 3 or worse hematological adverse events were less frequent in the lurbinectedin plus doxorubicin group than the control group( anemia, 57( 19) of 302 cases in the lurbinectedin plus doxorubicin group vs 110( 38) of 288 in the control group; neutropenia, 112( 37) vs 200( 69); thrombocytopenia, 42( 14) vs 90( 31)). The frequency of treatment-related adverse events leading to treatment termination was lower in the lurbinectedin plus doxorubicin group than in the control group( 26( 9) of 303 cases in the lurbinectedin plus doxorubicin group vs 47( 16) of 289 in the control group).
The results of the ATLANTIS trial indicate that the combination remedy of lurbinectedin plus doxorubicin didn’t ameliorate overall survival compared to the control in cases with regressed SCLC. Still, lurbinectedin plus doxorubicin showed a favorable hematological safety profile compared to the control.
Source: https://pubmed.ncbi.nlm.nih.gov/36252599/
Clinical Trial: https://clinicaltrials.gov/ct2/show/NCT02566993
Aix, S.P., Ciuleanu, T.E., Navarro, A., Cousin, S., Bonanno, L., Smit, E.F., Chiappori, A., Olmedo, M.E., Horvath, I., Grohé, C., Farago, A.F., López-Vilariño, J.A., Cullell-Young, M., Nieto, A., Vasco, N., Gómez, J., Kahatt, C., Zeaiter, A., Carcereny, E. and Roubec, J. (2023). Combination lurbinectedin and doxorubicin versus physician’s choice of chemotherapy in patients with relapsed small-cell lung cancer (ATLANTIS): a multicentre, randomised, open-label, phase 3 trial. The Lancet. Respiratory Medicine, [online] 11(1), pp.74–86. doi:https://doi.org/10.1016/S2213-2600(22)00309-5.