KEY TAKEAWAYS
- The study aimed to evaluate effects of ADCs vs other anti-HER2 therapies in pts with BC.
- The primary endpoints were PFS and OS.
- Researchers found that ADCs significantly improved PFS in HER2+ locally advanced or metastatic BC.
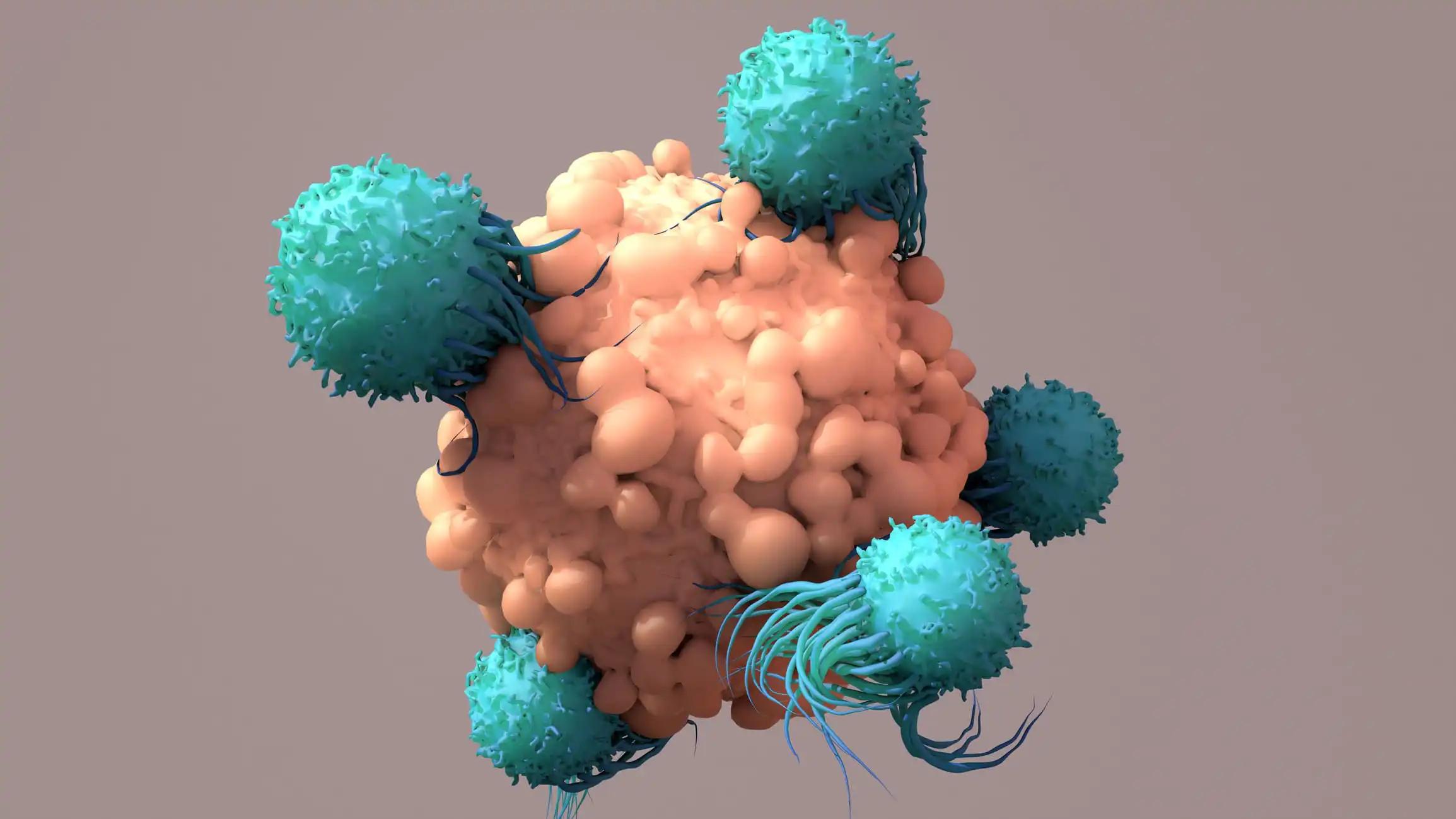
Novel antibody-drug conjugates (ADCs) offer a promising anti-cancer treatment, yet a stable and reliable treatment method is debated among clinicians.
Zian Kang and the team aimed to perform a meta-analysis to comparatively evaluate the effect of ADCs vs other anti-HER2 therapies on progression-free survival (PFS) and overall survival (OS) in treating HER2+ locally advanced or metastatic breast cancer (BC).
Researchers retrieved relevant randomized controlled trials (RCTs) from 5 databases involving 3870 patients (pts) and assessed bias risk using the Cochrane Collaboration’s tool via RevMan5.4 software. HR and 95% CIs were extracted to evaluate ADCs’ impact on PFS and OS in HER2+ advanced BC through meta-analysis.
They noted that significant improvements were observed in the ADCs subgroup, PFS (HR: 0.63, 95% CI: 0.49-0.80, P= 0.0002) and OS (HR: 0.79, 95% CI: 0.72-0.86, P< 0.0001) in pts with HER2-positive-locally advanced or metastatic BC.
The analysis indicated that PFS and OS were markedly prolonged in pts with prior exposure to HER2-targeted therapy. The reliability and stability of the results were validated by sensitivity analysis and publication bias assessments.
The findings proclaimed that antibody-drug conjugates significantly improved PFS in HER2+ locally advanced or metastatic BC, especially in those previously treated with HER2-targeted therapy, with stable and reliable results.
Funding was not applicable.
Source: https://pubmed.ncbi.nlm.nih.gov/38851684/
Kang, Z., Jin, Y., Yu H., et al. (2024). “Relative efficacy of antibody-drug conjugates and other anti-HER2 treatments on survival in HER2-positive advanced breast cancer: a systematic review and meta-analysis.” BMC Cancer. 2024 Jun 8;24(1):708. doi: 10.1186/s12885-024-12478-1. PMID: 38851684; PMCID: PMC11162572.