KEY TAKEAWAYS
- Phase 3 BYLieve study evaluated the ctDNA biomarkers based on prior CDK4/6 inhibitor treatment duration and PFS in patients with advanced breast cancer.
- Next-generation sequencing utilizing the PanCancer V2 Panel was used to identify ctDNA alterations.
- The outcome indicates that ALP and FUL combination therapy is effective and safe for patients with PIK3CA-mutated.
- Patients in the group with a ≤ 6-month duration had a lower median ctDNA fraction and fewer detected gene alterations than those in the group with a duration of>6 months.
- The study indicates that ALP and FUL combination therapy is effective and safe for patients with PIK3CA-mutated, hormone receptor-positive.
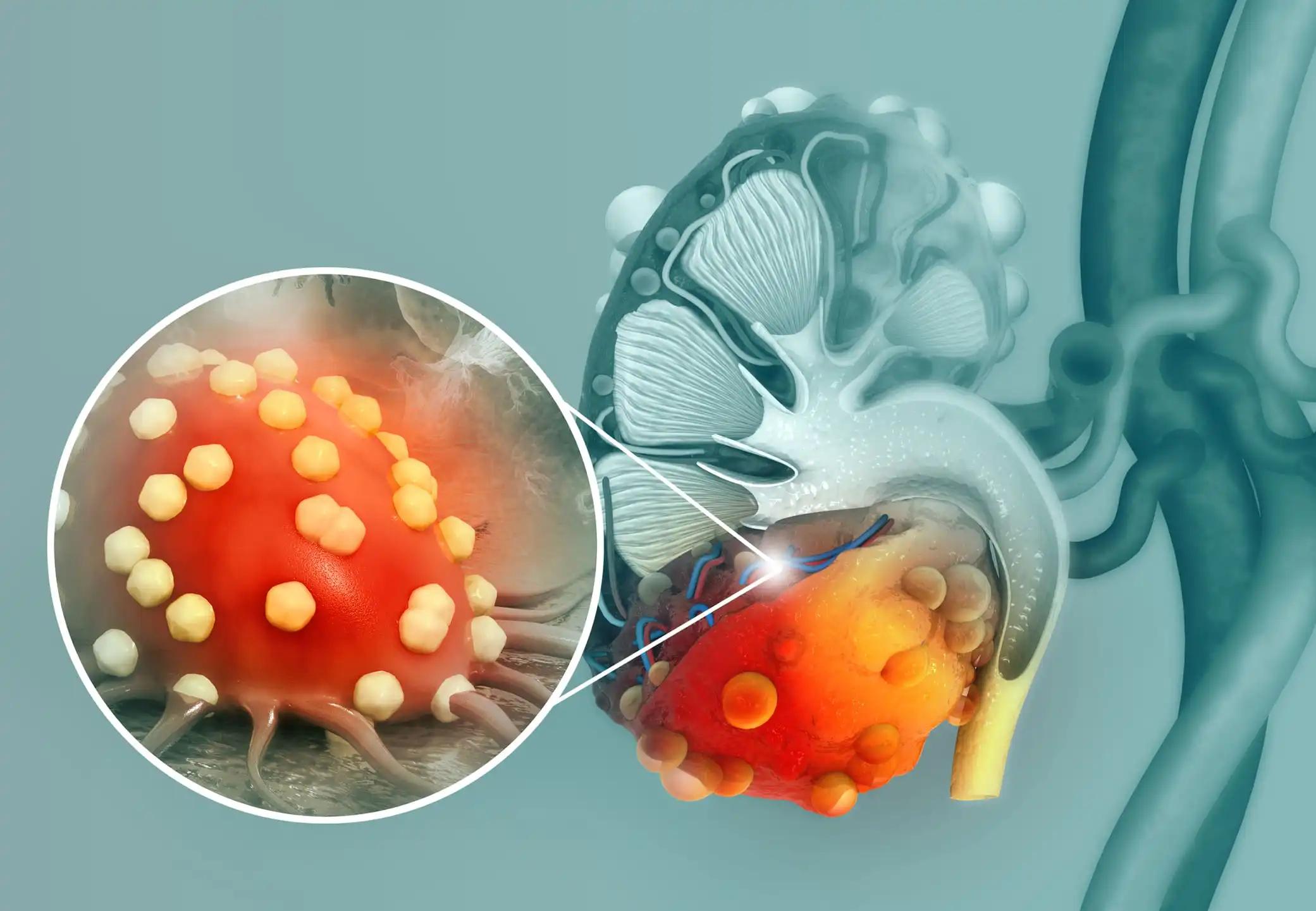
The combination of ALP, a selective inhibitor and degrader of PI3K-α, and fulvestrant (FUL) has been approved for patients diagnosed with hormone receptor-positive, HER2-negative advanced breast cancer and exhibiting a tumor mutation in PIK3CA, which is observed in approximately 40% of such patients. The primary analyses of the Phase 2 BYLieve study have indicated that the combination of ALP and ET is effective and safe for patients with PIK3CA-mutated, hormone receptor-positive, HER2-negative advanced breast cancer who have received prior CDK4/6 inhibitor treatment. Subsequent analyses, encompassing patients who experienced disease progression within six months of receiving CDK4/6 inhibitor and endocrine therapy treatment, validated the efficacy of ALP, irrespective of the duration of prior CDK4/6 inhibitor therapy. In this study, researchers evaluated the initial biomarkers in the circulating tumor DNA (ctDNA) based on the duration of prior CDK4/6 inhibitor treatment and progression-free survival (PFS) in patients with the BYLieve Cohorts A and B. The BYLieve study involved patients diagnosed with PIK3CA-mutated, hormone receptor-positive, and HER2-negative advanced breast cancer. The patients were divided into two cohorts, Cohort A and Cohort B.
Cohort A received a combination of CDK4/6 and aromatase inhibitors as their immediate prior treatment before being administered ALP and FUL. Cohort B, on the other hand, received CDK4/6 inhibitor and FUL before being given ALP and letrozole. At the designated data cutoff points, patients had a minimum follow-up of 18 months in Cohort A and 6 months in Cohort B. Patients were categorized into cohorts based on their previous CDK4/6 inhibitor treatment length, either less than or equal to six months or greater than six months. CTDNA alterations were identified via next-generation sequencing utilizing the PanCancer V2 Panel. The evaluation of PFS was conducted in every cohort and stratified by the length of previous CDK4/6 inhibitor treatment. Out of the total of 127 and 126 patients registered in Cohorts A and B, respectively, 98 patients (24 with a duration of less than or equal to 6 months and 74 with a duration of more than 6 months) and 94 patients (28 with a duration of less than or equal to 6 months and 66 with a duration of more than 6 months) were considered for this analysis. The selection was based on the availability of ctDNA samples, information on the duration of prior CDK4/6i, and centrally confirmed PIK3CA-mutated disease. The median progression-free survival (PFS) with a 95% confidence interval (CI) in this cohort was 8.2 months (5.6 – 9.5) and 5.6 months (3.7 – 7.1) in Cohorts A and B, respectively. In Cohort A, the median progression-free survival (95% confidence interval) was 12.0 months (5.5 to non-estimable) and 6.2 months (5.4 to 8.5) in the groups with less than or equal to 6 months and more than 6 months, respectively.
According to the OncoPrint genomic profiles, patients in the group with a ≤ 6-month duration had a lower median ctDNA fraction and fewer detected gene alterations, including those associated with ET and/or CDK4/6i resistance, as well as fewer amplifications of chromosomes 8/11, which are linked to early relapse, compared to those in the group with a duration of >6 months. The mPFS for Cohort B was observed to be 5.9 months (with a range of 3.5 to 11.0 months), while the ≤ 6-month and >6-month groups had mPFS of 5.6 months (with a range of 3.7 to 7.1 months) and 5.6 months (with a range of 3.7 to 7.1 months), respectively. Both cohorts exhibited elevated median circulating tumor DNA fractions and intricate tumor mutation profiles, indicative of a protracted therapeutic course. Cohort A, with a median ctDNA fraction and mutational complexity lower than the >6-month group, showed a slightly longer mPFS, suggesting a higher reliance on the mutant PI3K-α. In Cohort B, both the group with a disease duration of less than or equal to 6 months and the group with a disease duration of more than 6 months exhibited elevated median circulating tumor DNA fractions and comparable tumor mutation profiles. Further ctDNA and tissue analyses are required to clarify the association between ALP + ET effectiveness, treatment timing, and baseline genomic complexity.
Source: https://meetings.asco.org/abstracts-presentations/209428
Clinical Trail: https://clinicaltrials.gov/ct2/show/NCT03056755
Dejan Juric, Hope S. Rugo, Stephen K.L. Chia, Florence Lerebours, Manuel Ruiz-Borrego, Pamela Drullinsky, Eva M. Ciruelos, Patrick Neven, Yeon Hee Park, Christina H. Arce, Ennan Gu, Mukta Joshi, Estelle Roux, Murat Akdere, Nicholas C. Turner/Alpelisib (ALP) + endocrine therapy (ET) in patients (pts) with hormone receptor-positive (HR+), human epidermal growth factor receptor 2-negative (HER2–), PIK3CA-mutated (mut) advanced breast cancer (ABC): Baseline biomarker analysis and progression-free survival (PFS) by the duration of prior cyclin-dependent kinase 4/6 inhibitor (CDK4/6i) therapy in the BYLieve study/J Clin Oncol 40, 2022 (suppl 16; abstr 1018) DOI10.1200/JCO.2022.40.16_suppl.1018