KEY TAKEAWAYS
- The randomized, double-blind phase 3 trial (ROMAN) assessed the safety and efficacy of GC4419 and AVA to reduce the severity of OM due to CRT and cisplatin for LAHNC.
- AVA produced a statistically significant 16% relative reduction in OM incidence, 56% relative reduction in OM duration, and 27% relative reduction in grade 4 OM incidence compared to placebo.
- Treatment was well tolerated, with an adverse event profile consistent with expectations for CRT/cisplatin in LAHNC.
- AVA could reduce OM severity and duration and improve outcomes in LAHNC.
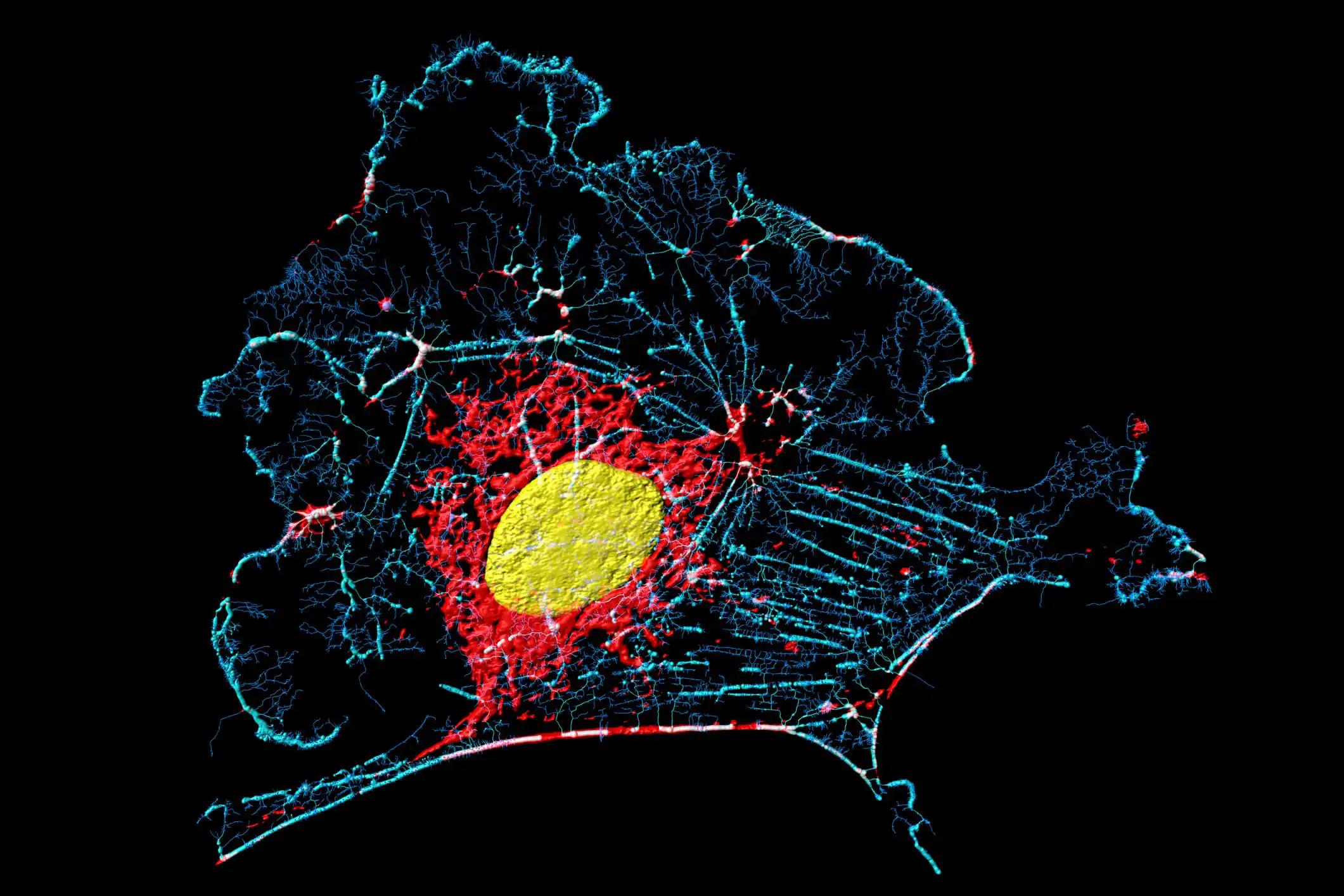
The combination of intensity-modulated radiation (IMRT) and cisplatin is a proven treatment for LAHNC; nevertheless, 70% of patients develop SOM (WHO grade 3 or 4), severely limiting their ability to eat solids (grade 3) or liquids (grade 4), and often necessitating sustenance through a feeding tube. Therefore, symptom control and palliative care are the mainstays of management (Elad 2020). So far, no medications have been developed or authorized by the FDA to treat SOM in LAHNC. Oral mucositis (OM) is caused by a surge of superoxide that is triggered by radiation therapy (RT) (Sonis 2004). Avasopasem (GC4419, AVA) is a selective small molecule dismutase mimic being studied for its potential to protect normal cells from radiation and potentially sensitize cancer cells to radiation by converting superoxide to hydrogen peroxide (Riley DP 2006, El-Mahdy 2020). Compared to placebo (PBO), AVA decreased the length and incidence of SOM caused by CRT for LAHNC in a randomized, double-blind phase 2b trial (Anderson 2019). For LAHNC of the Oral cavity (OC )or oropharynx(OP), the current trial (NCT03689712) evaluated the safety and effectiveness of AVA to lessen SOM caused by CRT.
Patients receiving 60-72 Gy of IMRT (>50 Gy to ≥2 oral mucosal sites) plus cisplatin (weekly or q3 weeks) were randomly assigned 3:2 to AVA 90 mg vs. PBO by 60-minute IV infusion, M-F before each RT fraction in a double-blind, placebo-controlled trial. Trained evaluators looked at OM on the WHO scale twice a month during RT and once a month for two months afterward. The primary outcome measures the Severity of Symptoms (WHO grades 3 or 4) through IMRT completion. The number of grade 4 OM episodes and the time SOM lasted for up to 2 weeks after IMRT were considered secondary outcomes.
The total sample size was 407 (241 AVA/166 PBO), with a median age of 61 and a composition of 86% male and 82% OP. There was a statistically significant reduction of 16% in the relative incidence of SOM (54% vs. 64%; p= 0.045) and a reduction of 56% in the relative duration of SOM (median, 8 vs. 18 days; p= 0.002). Statistically, there was a 27% drop in cases in fourth grade (p= 0.052). Several tertiary and exploratory objectives also showed improvement (table). There was no evidence of AVA-specific toxicity or a rise in cisplatin-attributable toxicity, and the incidence of adverse events (all grades, grade 3+, severe) was similar across treatment arms.
Overall, AVA was well tolerated, with an adverse event profile similar to that expected from IMRT/cisplatin in LAHNC. It was associated with statistically significant and clinically meaningful improvements in SOM compared to PBO across many parameters of SOM. For further details about the clinical trial, please visit NCT03689712.
Source: https://meetings.asco.org/abstracts-presentations/207129
Clinical Trial: https://clinicaltrials.gov/ct2/show/NCT03689712
J Clin Oncol 40, 2022 (suppl 16; abstr 6005), 10.1200/JCO.2022.40.16_suppl.6005