KEY TAKEAWAYS
- A phase 2 ALTN-03 trial aimed to assess the efficacy and safety of Anlotinib Plus Osimertinib in advanced NSCLC with EGFR T790M mutation after failure of prior EGFR TKIs.
- The primary endpoint was PFS. Secondary endpoints were ORR, DCR, OS, and AEs.
- The anlotinib-osimertinib combo shows promise for EGFR T790M mutation patients post-EGFR-TKI failure.
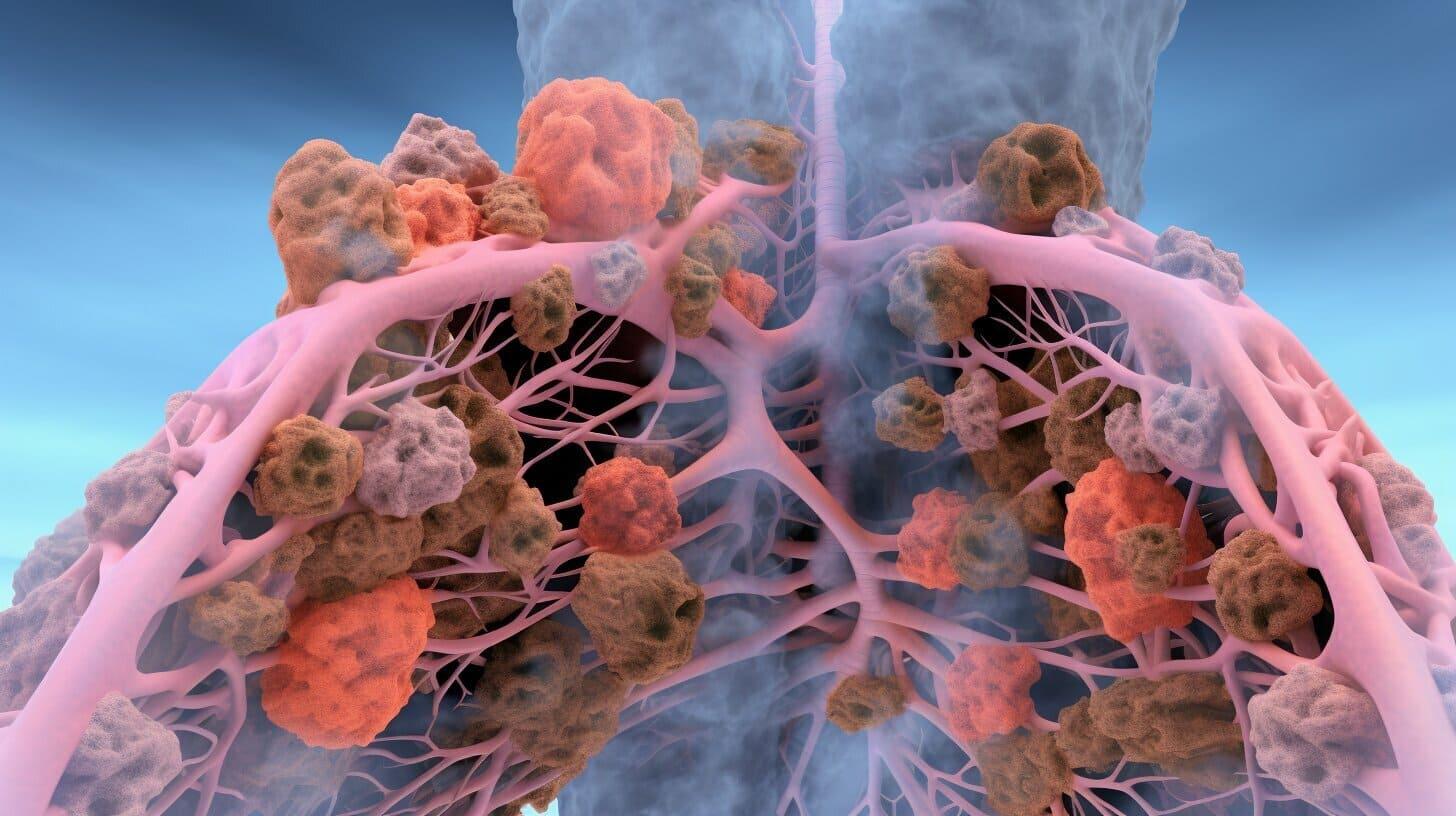
Despite the initial effectiveness of osimertinib in EGFR T790M resistance, subsequent acquired resistance occurs. Evaluating the involvement of the angiogenic pathway in EGFR-TKI resistance, researchers studied the safety and efficacy of combining osimertinib with anlotinib in advanced non-small cell lung cancer (NSCLC) cases showing confirmed EGFR T790M mutation post previous EGFR TKI treatment failure.
Researchers conducted a phase II clinical trial, treating NSCLC cases with EGFR T790M mutation with anlotinib (12mg daily for two weeks followed by a week off) and osimertinib (80mg daily within a 21-day cycle). The trial focused on progression-free survival (PFS) as the main goal, and secondary objectives included assessing objective response rate (ORR), disease control rate (DCR), overall survival (OS), and tracking adverse events (AEs). They also explored potential resistance biomarkers in circulating tumor DNA (ctDNA).
A total of 31 patients were treated with anlotinib and osimertinib from July 2019 to November 2021. As of August 31, 2022, they had a median follow-up of 27.7 months (IQR: 22.7-32.7). Median PFS was 16.7 months (95% CI 9.83-23.57). ORR was 48.4% (95% CI 30.6-66.6), and DCR was 100% (95% CI 86.3-100.0). AEs affected 15 patients (48.4%), with hypertension (22.6%) and leucopenia (12.9%) being the most common.
Analysis of ctDNA showed undetectable levels at Cycle 2 Day 21 linked to longer PFS compared to detectable ctDNA (not reached vs 8.8 months, HR 0.27, 95% CI 0.07-1.08; P=0.044). Decreased ctDNA was more prominent in patients with partial response (PR) or stable disease (SD) versus progressive disease (PD). Clearance of EGFR mutations in ctDNA after 6 weeks correlated with longer PFS (not reached vs 6.2 months, HR 0.10, 95% CI 0.03-0.35; P<0.001) and higher ORR (37.5% vs 9.1%; P=0.002).
Clearance of TP53 mutations after 6 weeks was also linked to longer PFS (not reached vs 8.8 months; P=0.010) and higher ORR (57.1% vs 20%; P=0.001). Among 22 patients with baseline T790M mutation, 19 (86.4%) lost T790M after treatment. Only 1 patient had C797S mutation with persistent T790M until disease progression. Other resistance mechanisms were noted, such as MET amplification, PIK3CA amplification, VEGFA amplification, and FGFR3 fusion.
Source: https://cattendee.abstractsonline.com/meeting/10925/presentation/2326
Clinical Trial: https://clinicaltrials.gov/ct2/show/NCT04029350/
R. Jiang1, X. Wang1, L. Wang1, D. Huang1, C. Ding2, C. Wang1
1Tianjin Medical University Cancer Institute & Hospital, Tianjin/CN ,2The Fourth Hospital of Hebei Medical University and Hebei Cancer Hospital, Shijiazhuang/CN