KEY TAKEAWAYS
- The clinical trial IMagyn050 (NCT03038100) aimed to assess the effectiveness of Atezo versus placebo in combination with carboplatin and CPB for front-line ovarian cancer patients.
- Tumor biomarkers, including CD8 density and location, immune inflamed phenotype, and immune-rich molecular subtype, are associated with overall survival.
- A prospective predictive biomarker was evaluated using PD-L1 IHC, CD8/PanCK IHC, and RNA-seq on FFPE tumors.
- The co-primary endpoints of PFS in ITT or PD-L1+ were not achieved. Patients with immune-inflamed tumors demonstrated a favorable overall survival benefit.
- The use of CPB decreased tumor proliferation and increased tumor immune inflammation, specifically in CD8 T cells, PD-L1, and IFNα/IFNγ response.
- The biomarkers PD-L1 and OXPHOS correlated with the therapeutic benefits of Atezo, irrespective of the anatomical site.
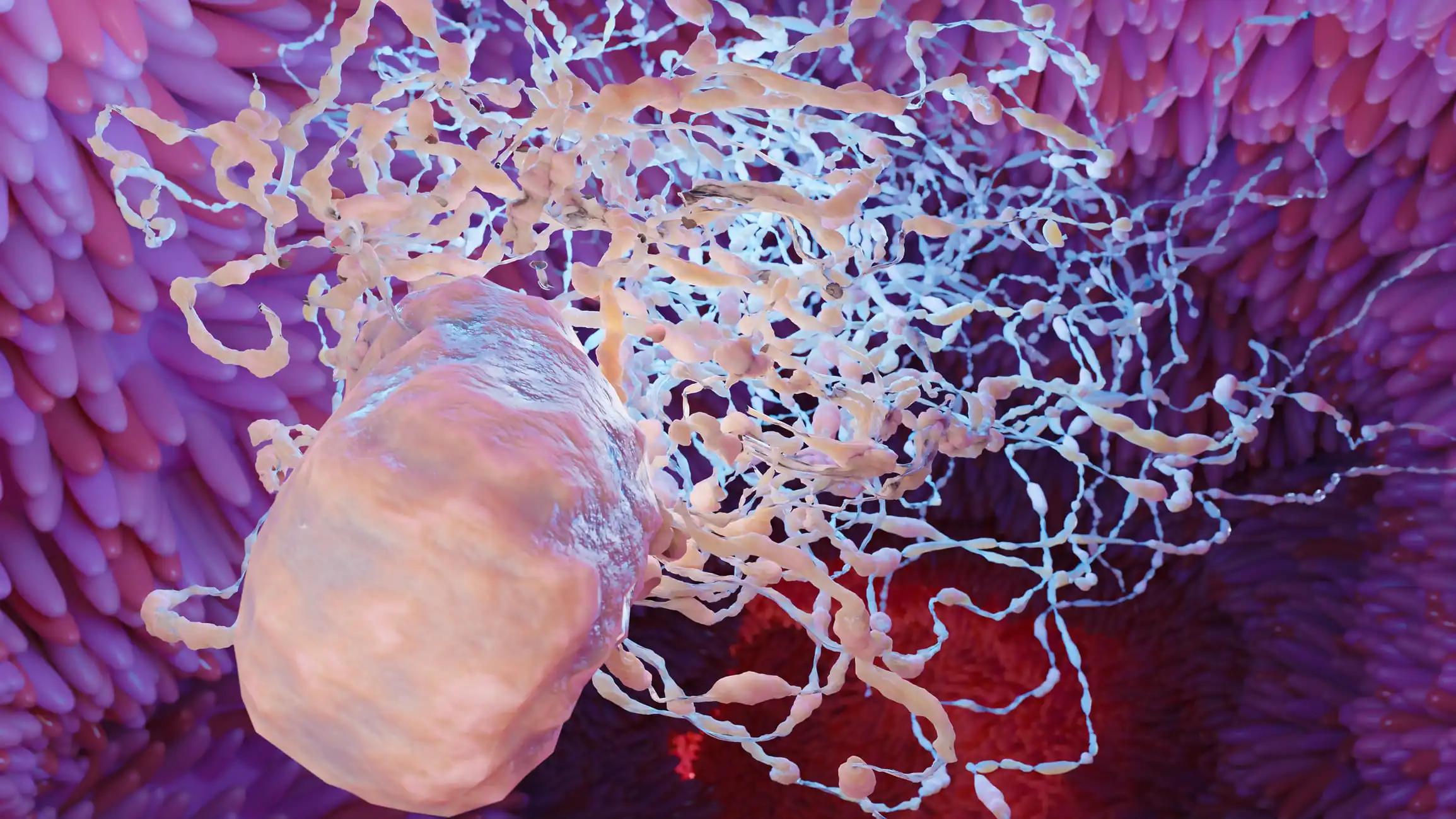
Tumor biomarkers, including CD8 density and location, immune inflamed phenotype, and immune-rich molecular subtype, have demonstrated associations with overall survival (OS) in various cancers treated with immune checkpoint blockade (ICB). The clinical trial IMagyn050 (NCT03038100) conducted an assessment on the effectiveness of Atezo versus placebo (Pla) in combination with carboplatin, paclitaxel, and bevacizumab (CPB) for front-line ovarian cancer patients (pts). The results revealed that the co-primary endpoints of PFS in ITT or PD-L1+ were not achieved (Moore et al. JCO 2021). The present IMagyn050 substudy evaluated prospective predictive biomarkers of tumor immunity for the clinical efficacy of Atezo. PD-L1 IHC, CD8/PanCK IHC, and RNA-seq were performed on FFPE tumors from the biomarker-evaluable population. The CD8 T cells and immune location phenotypes (inflamed, excluded, desert) were evaluated using CD8/PanCK IHC. Molecular subtypes, biological pathways, and cellular components (xCELL) were derived from RNA-seq data obtained from tissue samples at baseline (n=860), on-treatment (OT, 9 weeks, n=233), intra- (n=8) and inter-lesion (n=12) matched samples. A multivariate-adjusted Cox-regression analysis was conducted to assess predictive biomarkers, utilizing a hazard ratio (HR) interaction test for progression-free survival (PFS) and overall survival (OS).
Tumors that exhibit CD8 T cells, immunoreactive molecular subtypes, or an immune-inflamed phenotype were found to have a higher prevalence of PD-L1+. However, only patients with immune-inflamed tumors demonstrated a favorable overall survival benefit from Atezolizumab treatment, with a hazard ratio of 0.67. An enhanced progression-free survival (PFS) and overall survival (OS) benefit was noted in patients whose tumors exhibited high oxidative phosphorylation (OXPHOS, HR: 0.72/0.65) and UV response (UV, HR: 0.64/0.58) but not in those with IFNγ response. The aforementioned observations were made in relation to the administration of Atezo. The presence of plasma B cells was associated with a favorable overall survival benefit in patients treated with Atezolizumab compared to those who received a placebo (hazard ratio of 0.53). We utilized occupational therapy specimens obtained from patients in the neoadjuvant group to evaluate the impact of treatment on the tumor microenvironment. The analyses indicate that the use of CPB decreased tumor proliferation and increased tumor immune inflammation, specifically in CD8 T cells, PD-L1, and IFNα/IFNγ response.
The addition of Atezo further amplified these effects. Heterogeneous tumors pose a challenge in ovarian cancer regarding immune inflammation. The prevalence of tumor biomarkers exhibited variability based on anatomic locations, encompassing total CD8, CD8 localization, and molecular subtypes. The biomarker status within the same patient, inter- and intra-lesion, revealed that PD-L1 and plasma B cells were the most consistent. The molecular subtypes and immune phenotypes exhibited moderate intra-lesion agreement but were found to be discordant between lesions. The biomarkers PD-L1 and OXPHOS correlated with the therapeutic benefits of Atezo, irrespective of the anatomical site. This all-encompassing investigative analysis indicates that DNA harm, oxidative phosphorylation, plasma B lymphocytes, and immune-inflamed tumors, albeit not molecular subcategories or overall CD8 T lymphocytes, could potentially forecast the overall survival of patients treated with Atezolizumab and Tremelimumab. This therapeutic intervention stimulates immune-mediated inflammation within ovarian cancer neoplasms. It is noteworthy that several biomarkers exhibit significant heterogeneity. The results of this study underscore the difficulties in attaining long-lasting clinical advantages through targeted immunotherapy in patients with ovarian cancer.
Source: https://www.abstractsonline.com/pp8/#!/10828/presentation/3271
Clinical Trail: https://clinicaltrials.gov/ct2/show/NCT03038100
Venkatesh Krishnan, Ching-Wei Chang, Habib Hamidi, Michael A. Bookman, Charles Landen, Tashanna Myers, Hiroaki Kajiyama, Sakari Hietanen, Lyndsay Willmott, Premal Thaker, Cagatay Taskiran, Jalid Sehouli, Victor Khor, Yvonne Lin Liu, Sandro Pignata, Kathleen Moore, Luciana Molinero/Session MS.CL01.02 – Immune-based Biomarkers for Prognostic and Predictive Benefit
5702 – Ovarian cancer tumor microenvironment and atezolizumab (atezo) clinical activity: IMagyn050 sub-study/(2020). Abstractsonline.com. https://www.abstractsonline.com/pp8/#