KEY TAKEAWAYS
- The BRACELET-1 phase II trial aimed to evaluate the efficacy and safety of pelareorep plus paclitaxel in HR+/HER2- metastatic breast cancer pts.
- The primary endpoint was ORR. Secondary endpoints include PFS, OS, and toxicity.
- The study found combining pelareorep and paclitaxel was a promising treatment for HR+/HER2- metastatic breast cancer.
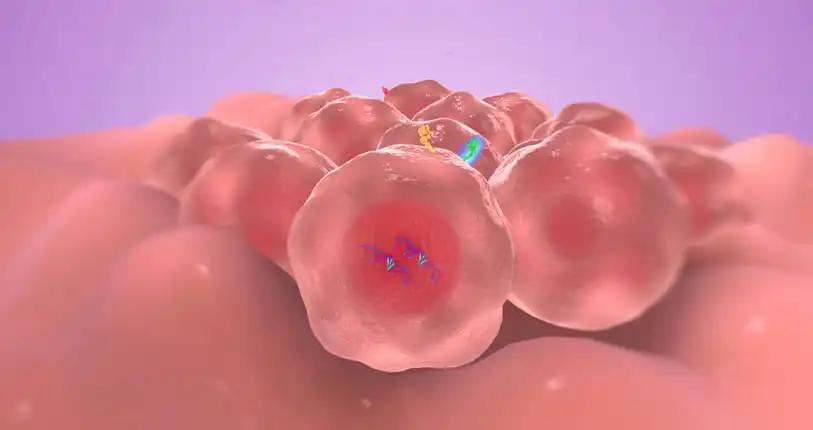
Pelareorep, an oncolytic reovirus, can create an inflamed tumor microenvironment (TME) in preclinical studies by increasing the number of tumor-infiltrating lymphocytes and PD-1/PD-L1 expression, potentially boosting the efficacy of immune checkpoint blockade. Pelareorep can create an inflamed TME in preclinical studies, which may improve the efficacy of immune checkpoint blockade.
Researchers aimed to evaluate the efficacy and safety of pelareorep plus paclitaxel (PTX) in patients(pts) with HR+/HER2- metastatic breast cancer.
The study included pts with HR+/HER2- metastatic breast cancer who had previously experienced disease progression on at least one hormonal therapy with a CDK4/6 inhibitor. Following a safety assessment for Cohort 3, pts were randomly assigned in a 1:1:1 ratio to three groups, PTX alone (Cohort 1), PTX + pelareorep (Cohort 2), or PTX + pelareorep + avelumab (Cohort 3). The primary endpoint was to assess the overall response rate (ORR) at week 16 using RECIST v1.1 criteria without formally comparing the groups. Secondary endpoints included evaluating toxicity, progression-free survival (PFS), and overall survival (OS) and analyzing blood samples collected at different treatment cycles C1D1, C2D1, and C4D1, with T-cell receptor sequencing performed.
About 48 pts were enrolled, with a median age of 55.5 years (37-74). Among them, 83% had visceral disease, and a small percentage had prior exposure to everolimus or alpelisib (12%). Approximately 27% had received taxanes in the neo/adjuvant setting, 3 pts withdrew consent before treatment, and 2 discontinued after one week, considered non-responders for PFS. Common pelareorep-related side effects included fever, chills, and flu-like infusion reactions, with 15% of pts requiring hospitalization, despite acetaminophen prophylaxis. About 33% discontinued pelareorep, and 35% discontinued avelumab due to toxicity. Pelareorep led to increased turnover in T-cell repertoire, with the identification and expansion of new and existing T-cell clones by Cycle 2, Day 1.
The study found combining pelareorep and paclitaxel was a promising treatment for HR+/HER2- metastatic breast cancer. Still, monitoring pts for toxicity and providing supportive care is important.
Source: https://ascopubs.org/doi/abs/10.1200/JCO.2023.41.16_suppl.1012
Clinical Trial: https://classic.clinicaltrials.gov/ct2/show/NCT04215146
Amy Sanders Clark, Fengmin Zhao, Paula Klein, Alberto J. Montero, Carla Isadora Falkson, Elisa Krill-Jackson, Kendrith M. Rowland, Sagar D. Sardesai, Jason Anthony Incorvati, Patrick Michael Dillon, Antonio C. Wolff, Houra Loghmani, Richard Trauger, Thomas Charles Heineman, Matthew C. Coffey, and Kathy Miller. DOI: 10.1200/JCO.2023.41.16_suppl.1012 Journal of Clinical Oncology 41, no. 16_suppl (June 01, 2023) 1012-1012.