KEY TAKEAWAYS
- The phase 3 GAIA/ CLL13 trial compared 3 time-limited venetoclax- grounded rules with chemoimmunotherapy in treatment- naïve cases with habitual lymphocytic leukaemia.
- Chromosome banding analyses with IL- 2/ CpG- stimulation showed high karyotypic complexity (hCKT; ≥ 5 chromosomal rarities) was associated with poor prognostic in all treatment arms.
- Translocations were singly linked to worse progression-free survival across all treatment arms.
- Karyotyping at progression revealed increased genomic complexity following chemoimmunotherapy compared to venetoclax- grounded rules.
- These results suggest that hCKT and translocations are associated with poor issues in CLL cases treated with venetoclax- grounded time-limited combinations.
In cases with chronic lymphocytic leukaemia( CLL) treated with chemoimmunotherapy( CIT), the presence of ≥ 3( complex karyotype, CKT) and specifically ≥ 5( high- CKT, hCKT) chromosomal rarities( CA) is associated with a poor prognostic. Examinations into the prognostic impact of CKT with targeted agents are miscellaneous and disagreeing, with reports of danger and no effect on progression-free( PFS) and overall survival(zilch). We prospectively estimated the impact of CKT in a large cohort of cases treated with venetoclax( ven)- grounded time-limited combinations within the GAIA/ CLL13 trial.
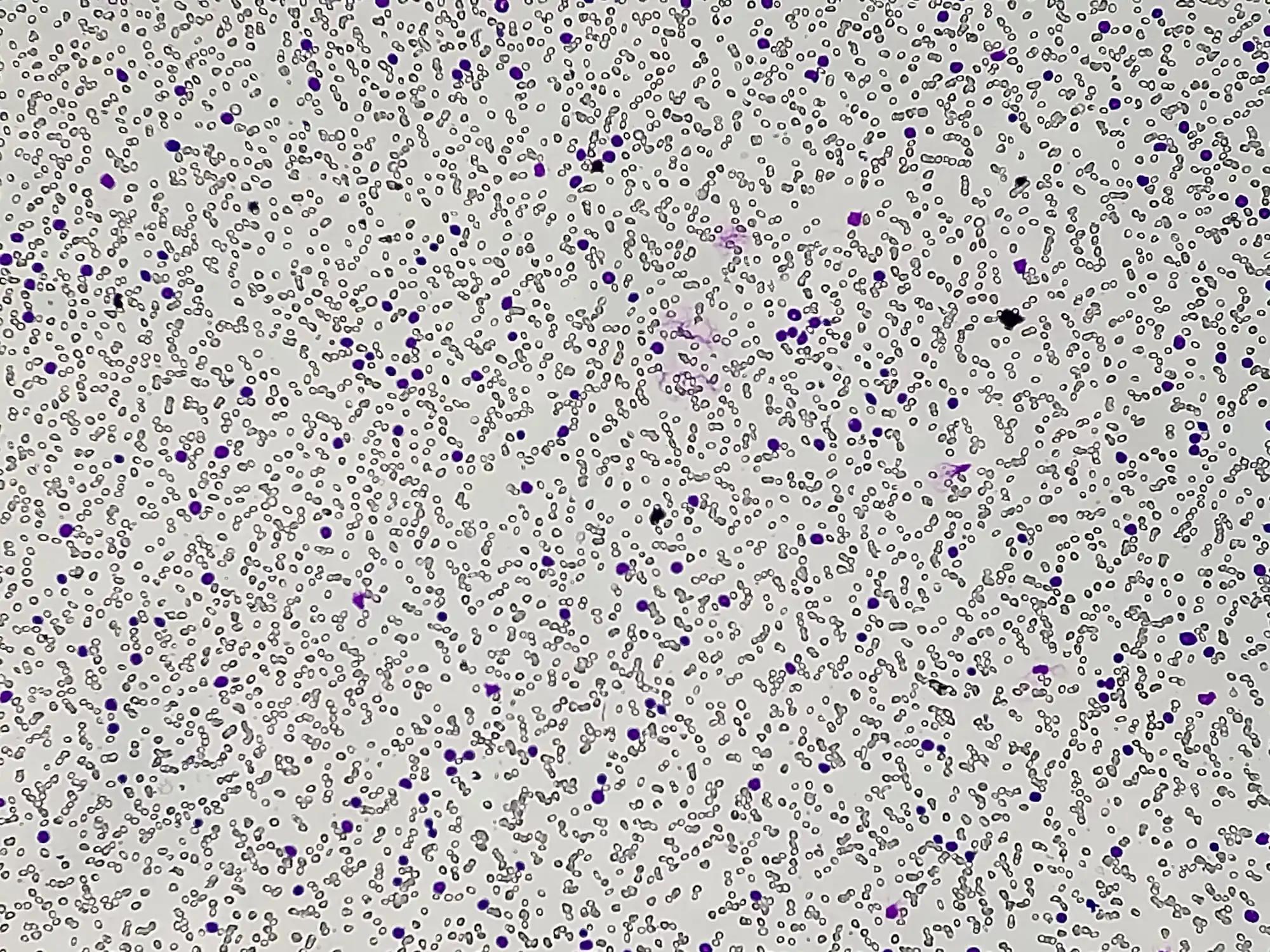
Chromosome banding analyses were performed following IL- 2/ CpG- stimulation, and karyotypes were anatomised according to ISCN 2020. Of the 895 cases, 672 were in the pooled ven population and 223 in the CIT arm. No CKT( nCKT) was linked in79.4,81.0,83.5, and87.9 of cases treated with CIT, RVe, GVe, and GIVe independently, while intermediate CKT( iCKT) and hCKT were set up in13.5,14.7,11.5,9.4 and7.2,4.3,5.0 and2.7, independently. manly gender, del( 11q), del( 6q) and trisomy 12 were linked to CKT. At month 15, undetectable MRD( uMRD) rates were lower in cases with CKT compared to nCKT in the CIT arm(37.0 vs57.1; OR0.44, p = 0.016).
Across all treatment arms, those with ≥ 5 CA had significantly shorter PFS than those with< 5 CA. With CIT, iCKT was also associated with shorter PFS( vs nCKT HR2.49, p = 0.003). In none of the ven arms, still was a significant PFS difference between iCKT and nCKT. Translocations( TL) were associated with inferior PFS, anyhow of the treatment arm. In the ven-treated population, this difference was driven substantially by unstable TL( vs no TL HR3.83, p<0.001), but balanced TL still conferred inferior PFS compared to those without any
TL( HR1.66,p = 0.035). Cases with CKT but without TL had similar PFS to nCKT( HR0.53, p = 0.217), while those with
CKT and TL had significantly shorter PFS( HR2.79, p<0.001). In a multivariate analysis, CKT was linked as an independent prognostic factor for PFS with CIT.
In discrepancy, only hCKT and TL were linked as independent adverse factors for PFS in pool even. zilches was shorter for CKT vs nCKT with CIT( HR3.25, p = 0.044), but not in the ven arms. At progression( PD), karyotyping data was available in 88 of 161(54.7) cases. With CIT, 7 of 20(35.0) cases with CKD at birth acquired CKT at PD, while in the pooled ven group, this bit was mainly lower(6/45,13.3). This study confirms the adverse impact of CKT with CIT and identifies hCKT as a negative prognostic factor in the environment of ven-grounded combination treatment in CLL. Translocations were associated with inferior PFS in all treatment arms, while increased genomic complexity was observed following CIT as opposed to ven-grounded treatments.
Source:https://ash.confex.com/ash/2022/webprogram/Paper164786.html
Clinical trial:https://clinicaltrials.gov/ct2/show/NCT02500407
Moritz Furstenau, MD1, Yvonne Thus2*, Sandra Robrecht, PhD3*, Clemens Mellink4*, Anne-Marie Van Der Kevie-Kersemaekers5*, Julie M.N. Dubois, MD, PhD6*, Julia Von Tresckow, MD7*, Michaela Patz8*, Michael Gregor, MD9*, Patrick Thornton, MB, FRCPath10*, Philipp B. Staber, MD, PhD11, Tamar Tadmor, MD12*, Mark-David Levin13, Caspar Da Cunha-Bang, MD, PhD14, Christof Schneider, MD15*, Christian Bjørn Poulsen, MD16*, Thomas Illmer, MD17, Björn Schöttker18*, Ann Janssens, MD, PhD19*, Ilse Christiansen20*, Michael Baumann, MD21*, Thomas Noesslinger, MD22, Josien Regelink, MD23*, Ellen C Dompeling24*, Vesa Lindström, MD25*, Gunnar Juliusson, MD, PhD26, Anouk Widmer27*, Jeroen Simon Goede28*, Neta Goldschmidt, MD29*, Florian Simon, MD1*, Nisha De Silva, MBBS, MRCP, FRCPath30*, Anna-Maria Fink, MD31*, Kirsten Fischer, MD30*, Clemens-Martin Wendtner32, Matthias Ritgen, MD33*, Monika Brüggemann, MD34*, Eugen Tausch, MD35, Stephan Stilgenbauer, MD36, Eric Eldering, PhD37*, Carsten Utoft Niemann, MD, PhD38, Michael Hallek, MD39,40, Barbara Eichhorst, MD41, Karl-Anton Kreuzer, MD1* and Arnon P. Kater, MD, PhD42