KEY TAKEAWAYS
- The phase 1 trial aimed to identify prognostic mutations in AML/MDS.
- The results demonstrated that early magrolimab shrinks TP53 mutations in MDS/AML, opening a potential path for new cancer treatments.
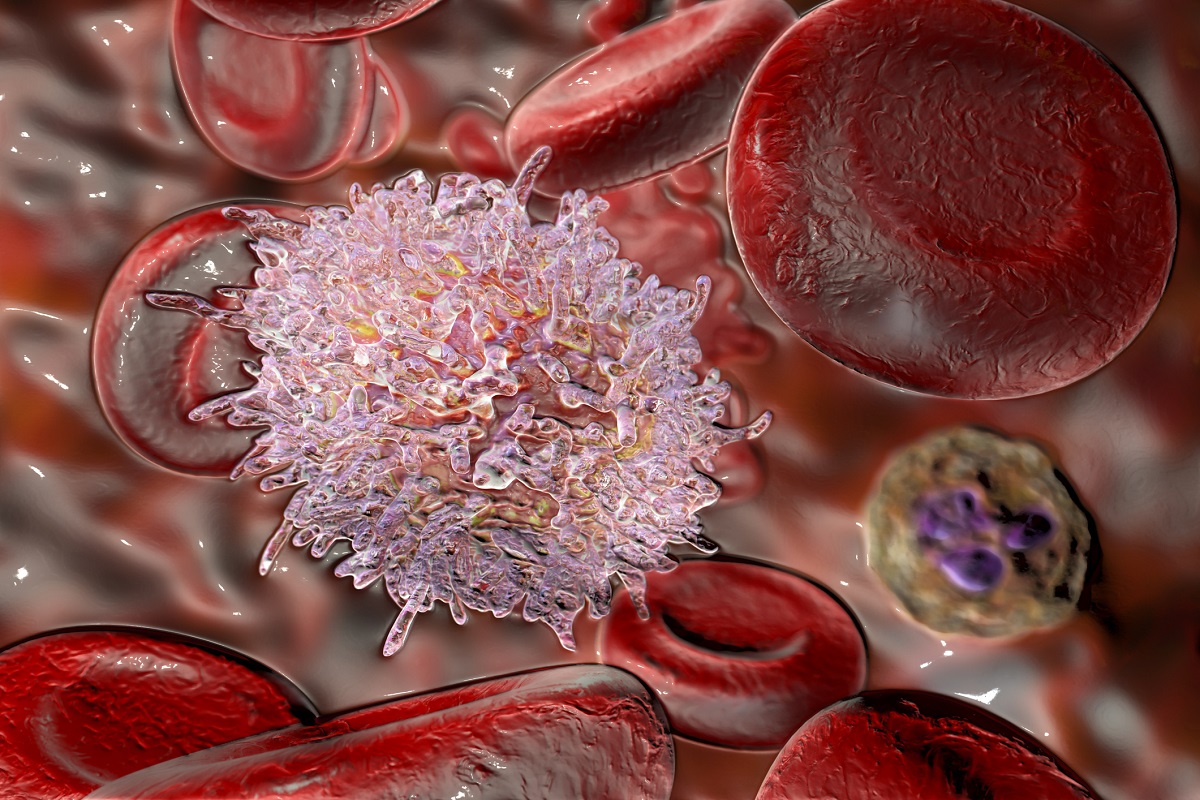
Magrolimab, an anti-CD47 monoclonal antibody, interrupts tumor antiphagocytic signals, aiding immune-driven eradication of cancer cells. Azacitidine, recognized for amplifying tumor cell prophagocytic signals, synergizes with magrolimab to enhance the immune system’s ability to engulf and eliminate cancerous cells. This dual strategy shows promise in advancing cancer immunotherapy by concurrently blocking inhibitory signals and promoting phagocytosis.
Lisa Johnson and her researchers spearheaded the study that aimed to investigate the prognostic impact of somatic mutations in patients with Acute Myeloid Leukemia (AML) (n=23) or Mutant Myelodysplastic Syndromes (MDS) (n=56) treated with the synergistic combination of magrolimab, an anti-CD47 antibody-blocking tumor antiphagocytic signals) and azacitidine enhancing tumor pro-phagocytic signals.
In the interventional study, patients underwent escalating magrolimab doses (1–30 mg/kg) for 2 weeks, followed by maintenance at 30 mg/kg weekly or biweekly from Cycle (C) 3, along with azacitidine (75 mg/m2) on days (D) 1–7 of each 28-day cycle. Whole-exome sequencing was conducted on screening and post-treatment bone marrow aspirates from treatment-naive patients with Revised International Prognostic Scoring System (IPSS-R) higher-risk MDS and AML patients ineligible for induction therapy. Processing pipelines, integrating algorithms with novel filtering, curation, and quality-control steps, were developed using a variant allele frequency (VAF) cutoff of 0.0
The result demonstrated that at screening, TP53 emerged as the predominant variant (MDS: 8/51 [16%]; median VAF [range]: 0.38 [0.14–0.86]; AML: 22/35 [63%]; median VAF [range]: 0.37 [<0.07–0.88]). 63% of MDS patients (5/8) and 59% of AML patients (13/22) exhibited complex cytogenetics. TP53 biallelic loss (2 mutations, mutation+alt 17, or VAF >0.5) occurred in 5 MDS patients and 17 AML patients. In the MDS subgroup, TP53-mutated patients showed 38% complete remission (CR) and 13% marrow CR (mCR) rates, while TP53 wild-type patients displayed 30% CR (13/43) and 35% mCR (15/43).
All three TP53-mutated CR patients had a TP53 VAF <0.07 by C5D1. In the AML group, CR rates for TP53-mutated and wild-type patients were 59% (13/22, including 2 with CR with incomplete/partial hematologic recovery and 1 with morphologic leukemia-free status) and 46% (6/13), respectively. Among TP53-mutated CR patients, TP53 VAF <0.07 was observed in 7/13 (54%) patients at C3D1, 9/12 (75%) at C5D1, and 3/5 (60%) at C7D1. Comparable CR rates (MDS, 20%–50%; AML, 33%–100%) were noted in non-TP53 mutated patients, generally with lesser VAF decreases.
The study concluded that the number of patients with MDS or AML receiving magrolimab combined with azacitidine and magrolimab treatment as early as cycle 3 decreased the proportion of cancer cells carrying TP53 mutations. It also suggested the potential of magrolimab to change the course of disease in malignancies with TP53 mutations. The study was sponsored by Gilead Sciences.
Source: https://clml-soho2023.elsevierdigitaledition.com/362/index.html
Clinical Trial: https://clinicaltrials.gov/study/NCT03248479
Johnson L, Zhang Y, Li B, et al. “Nature of Clinical Response and Depth of Molecular Response in Patients With TP53‑Mutant Myelodysplastic Syndromes (MDS) and Acute Myeloid Leukemia (AML) Treated With Magrolimab With Azacitidine” Presented at SOHO 2023. (Abstract: MDS-345)