KEY TAKEAWAYS
- The phase III IMagyn050 trial demonstrated that genomic instability brought on by BRCA1/2 mutation or HRD is not linked to increased sensitivity to immune checkpoint inhibitors.
- In this two-arm study, participants were given Atezolizumab With Paclitaxel, Carboplatin, and Bevacizumab, while the other arm received Placebo With Paclitaxel, Carboplatin, and Bevacizumab.
- The primary outcome measure of the trial was Progression-Free Survival.
- Low TMB in ovarian tumors with BRCA1/2 mutations or HRD, no enhanced atezolizumab benefit.
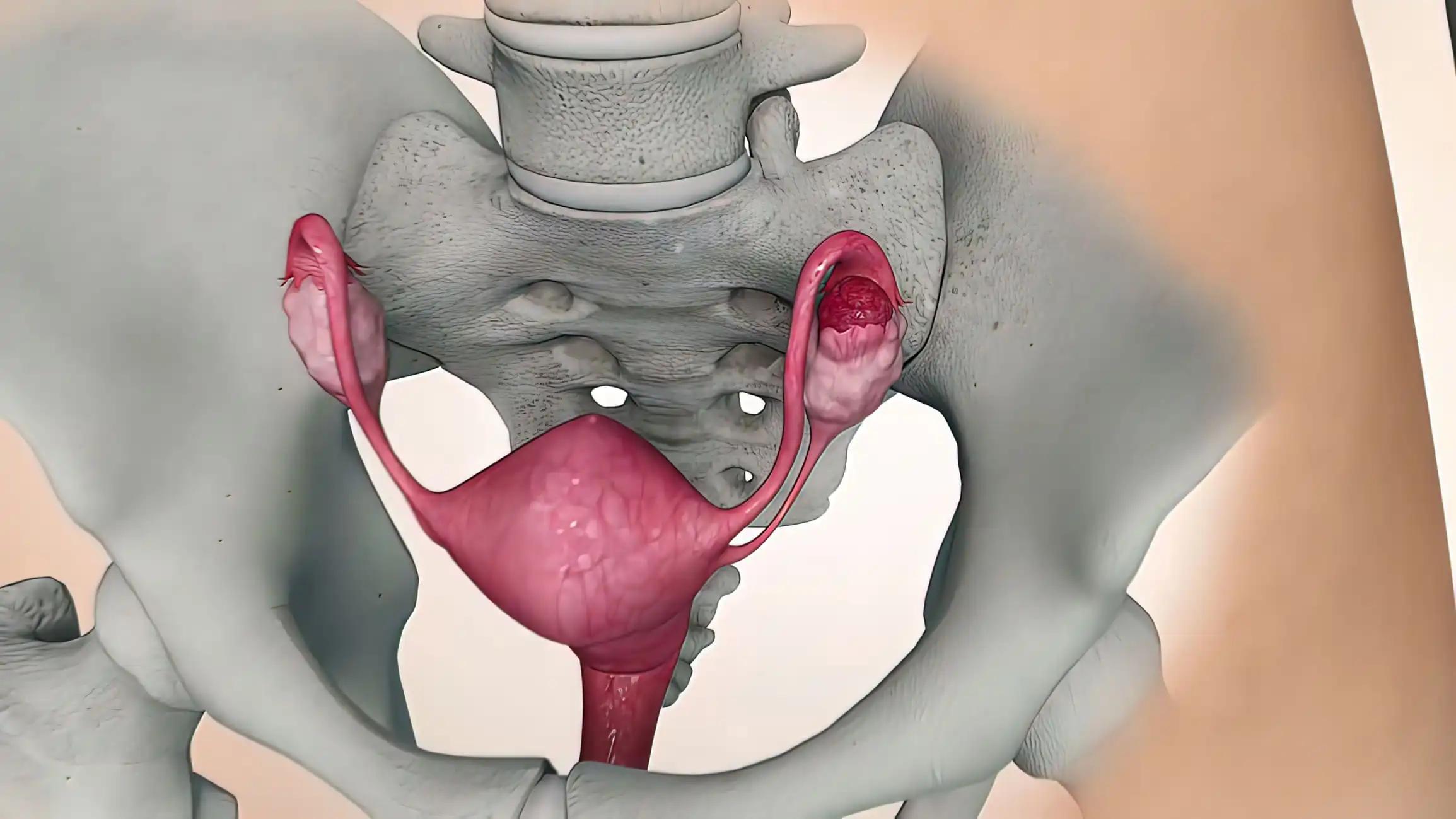
The Phase III of IMagyn050 trial was conducted to determine whether Atezolizumab was beneficial for individuals with BRCA1/2-mutated or homologous recombination-deficient (HRD) ovarian cancer.
Patients with recently discovered ovarian cancer were randomly assigned to receive either Atezolizumab or a placebo, in addition to standard chemotherapy and Bevacizumab. VENTANA SP142 assay was used to centrally define PD-L1 status of immune cells infiltrating tumors, and the FoundationOne test was used to assess genomic alterations, such as harmful BRCA1/2 mutations, genomic loss of heterozygosity (gLOH), tumor mutation burden (TMB), and microsatellite instability (MSI). Regardless of the presence of BRCA1/2 mutations, HRD was classified as gLOH 16%. Using conventional correlation studies and the log-rank of Kaplan-Meier estimates, it was determined whether there might be any relationships between progression-free survival (PFS) and genomic biomarkers.
22% (234/1050) of samples with biomarker-evaluable samples had BRCA1/2 variants, and 46% (446/980) had HRD. Regardless of BRCA1/2 or HRD, the median TMB was minimal. Just 3% (29/1024) of samples had TMB 10 mut/Mb, and 0.3% (3/1022) had elevated MSI. PFS was higher in HRD tumors compared to proficient tumors and in BRCA2-mutated tumors compared to BRCA2-non-mutated tumors. In contrast to BRCA1/2 mutations, HRD was linked with PD-L1 positivity (1% expression on immune cells). In BRCA2-mutated or HRD tumors, PFS was not improved by adding atezolizumab; however, there was a trend towards better PFS with atezolizumab in BRCA1-mutated tumors.
Despite BRCA1/2 mutations or HRD, the majority of ovarian tumors have minimal TMB. Atezolizumab benefits were not expected to increase by BRCA1/2 mutation or HRD. In ovarian cancer, this is the first randomized, double-blind study to show that genomic instability brought on by BRCA1/2 mutation or HRD is not linked to increased sensitivity to immune checkpoint inhibitors.
Source: https://aacrjournals.org/clincancerres/article/doi/10.1158/1078-0432.CCR-22-2032/716136/Influence-of-Genomic-Landscape-on-Cancer
Clinical Trial: https://clinicaltrials.gov/ct2/show/NCT03038100
Landen, C. N., Molinero, L., Hamidi, H., Sehouli, J., Miller, A., Moore, K. N., Taskiran, C., Bookman, M., Lindemann, K., Anderson, C., Berger, R., Myers, T., Beiner, M., Reid, T., Van Nieuwenhuysen, E., Green, A., Okamoto, A., Aghajanian, C., Thaker, P. H., Blank, S. V., Khor K. V., Chang C.W., Lin G. Y., & Pignata, S. (2023). Influence of Genomic Landscape on Cancer Immunotherapy for Newly Diagnosed Ovarian Cancer: Biomarker Analyses from the IMagyn050 Randomized Clinical Trial. Clinical cancer research : an official journal of the American Association for Cancer Research, CCR-22-2032. Advance online publication. https://doi.org/10.1158/1078-0432.CCR-22-2032