KEY TAKEAWAYS
- The IRIS trial aimed to decipher the mechanisms of resistance to immunotherapy in cancer.
- Tumor biopsies and blood samples from solid tumor pts were sequenced to identify genomic and transcriptomic changes associated with ICI resistance.
- The study found early ICI-resistant cancers exhibited EMT, cell de-differentiation, and CAF features, suggesting these may drive progression.
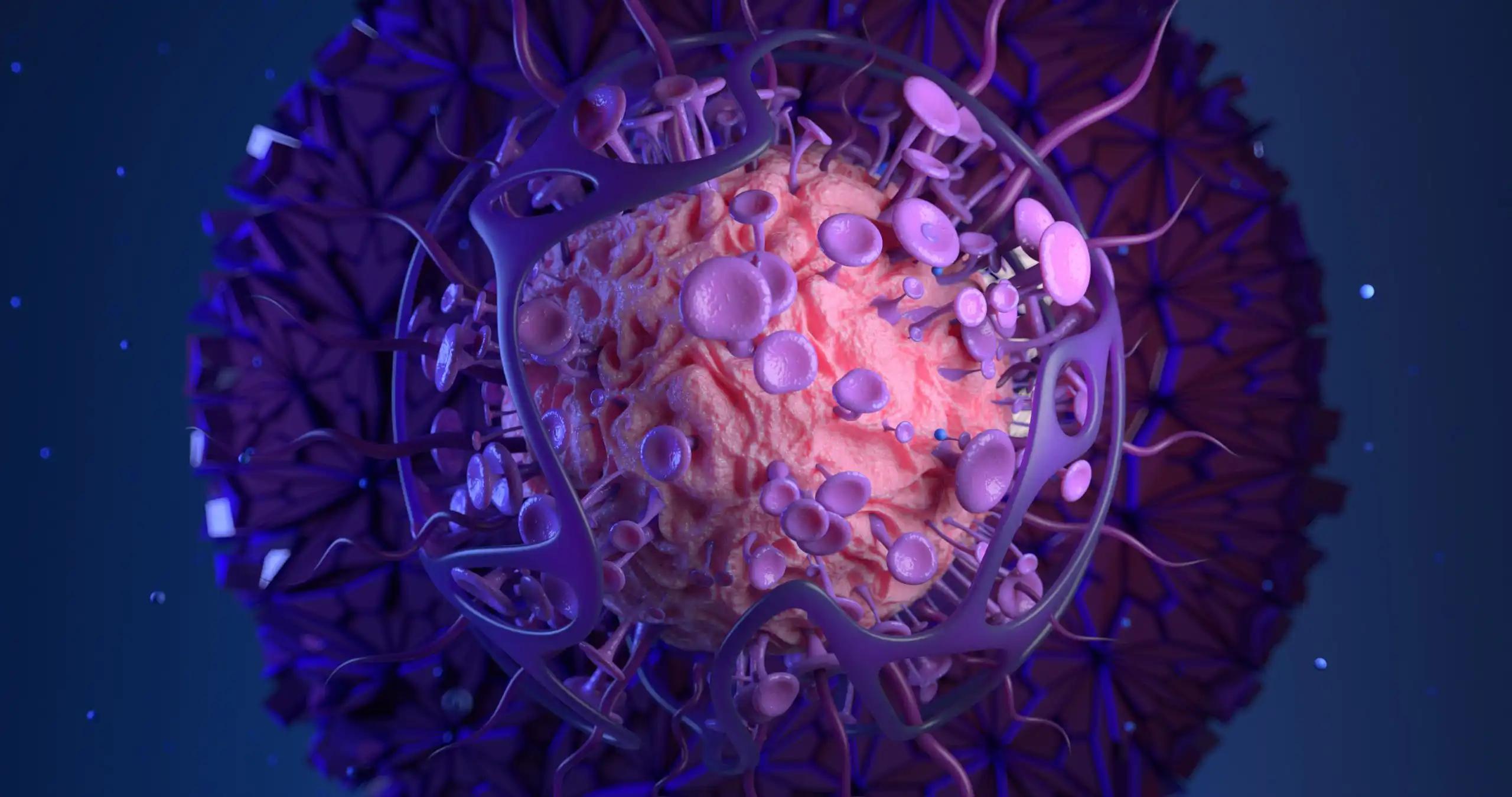
Most cancer patients(pts) have limited or no response to anti-PD1/PD-L1 immunotherapy. Whole genome and transcriptome analysis (WGTA) could help understand why some cancers resist immunotherapy and find new ways to predict which pts will respond.
Researchers aimed to decipher the mechanisms of resistance to immunotherapy in cancer.
Fresh tumor biopsies and blood samples were obtained from solid tumor pts during disease progression while undergoing treatment with immune checkpoint inhibitors (ICI). DNA and RNA were extracted from the tumor tissue, and paired blood samples were sequenced using an Illumina NovaSeq6000 system (2×150 paired reads for WG and 2X100 paired reads for WT). Various analyses were conducted, including assessing copy number alterations (CNAs), structural variants (SVs), mutation signatures, and gene expression. Wald tests in univariable and multivariable logistic regression models were used to compare these factors.
About 73 pts (45 Primary(Pr)/28 Acquired(Ar)) were included in the study. WGTA was conducted in 22 pts(14 Pr/8 Ar). Key patient characteristics included a median age of 60.5 years (range 26-79), 68% male and 32% female. Tumor types comprised 50% melanoma, 36% squamous cell carcinoma of the head and neck, and 14% other tumor types. Treatment distribution was 41% PD-1/PD-L1 inhibitor monotherapy and 59% PD-1/PD-L1 inhibitor combinations. There were no significant differences in median tumor mutation burden (TMB, coding; 2.8, range 0.6-30.5 for Pr vs 4.4, range 1.6-12.8 for Ar), the median percentage of the genome altered by copy number alterations (CNA) (43% Pr vs 65% Ar), or a median number of SVs(144, range 9-775, for Pr vs 76, range 25-924, for Ar pts). Following RNA sequencing, there was a significant increase in the expression of the epithelial-mesenchymal transition (EMT) hallmark gene set from msigDB and three previously reported ICI-resistance gene expression signatures in Pr compared to Ar pts (P≤0.05) in univariable analysis.
The analyzed signatures included genes related to the regulation of EMT, cellular de-differentiation, and a cancer-associated fibroblast (CAF) signature (IPRES signature, Hugo et al. Cell 2016; melanocytic plasticity signature [MPS], Pérez-Guijarro et al. Nat Med 2020; LRRC15 CAF signature, Dominguez et al. Cancer Discov. 2020). When accounting for cancer type, the MPS signature was found to have a significant association with resistance to Pr versus Ar resistance in multivariable analysis (P= 0.048).
The study found early ICI-resistant cancers exhibited EMT, cell de-differentiation, and CAF features, suggesting these may drive progression.
Source: https://ascopubs.org/doi/abs/10.1200/JCO.2023.41.16_suppl.2602
Clinical Trial: https://clinicaltrials.gov/study/NCT04243720
Sofia Genta, Jeff Bruce, Xuan Li, Sam Felicen, Albiruni Ryan Abdul Razak, Samuel Saibil, Marcus O. Butler, Philippe L. Bedard, Bernard Lam, Ming Sound Tsao, Wey Liang Leong, Alexandra Easson, Ben X Wang, Ilinca Lungu, David Paul Goldstein, Aaron Richard Hansen, Lawson Eng, Trevor John Pugh, Lillian L. Siu, and Anna Spreafico. DOI: 10.1200/JCO.2023.41.16_suppl.2602 Journal of Clinical Oncology 41, no. 16_suppl (June 01, 2023) 2602-2602.