KEY TAKEAWAYS
- Phase III DALIAH (NCT01387763) was a 5-arm, randomized study exploring better treatment options for Philadelphia Chromosome Negative (Ph-)Chronic Myeloid Neoplasms.
- The study investigated the association between complete (CHR) and molecular response in MPN patients treated with cytoreductive therapy.
- The study’s primary measure was the molecular response in terms of changes from baseline by assessing qPCR according to the ELN guidelines.
- The study found that the mutations in TET2, DNMT3A, or ASXL1 were significantly associated with prior stroke in MPN patients.
- Different mutations in MPN patients may require different treatment approaches to optimize patient outcomes.
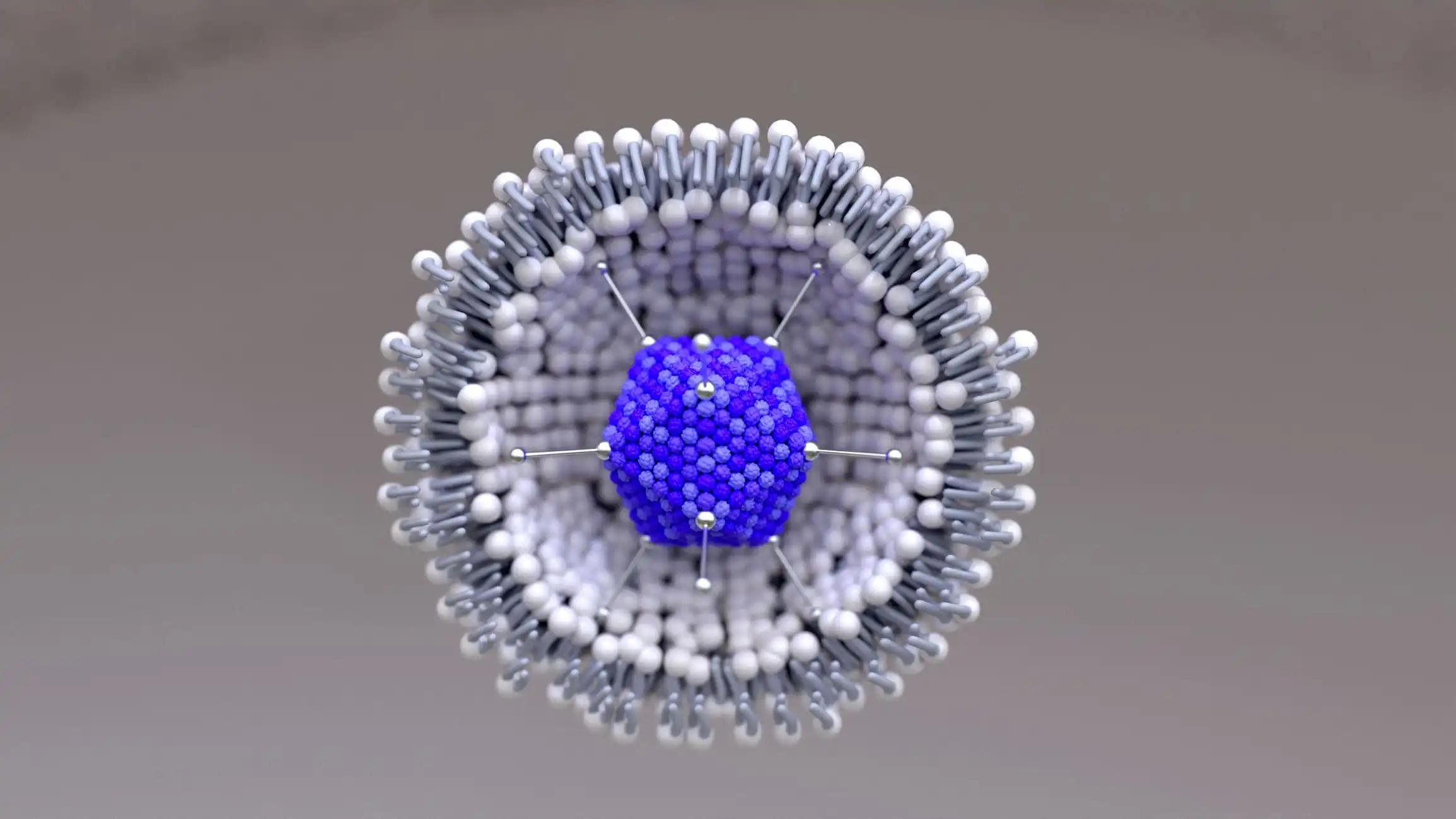
The Phase III DALIAH study discussed the impact of somatic mutations on the molecular response to cytoreductive treatment in patients with myeloproliferative neoplasms (MPNs). Myeloproliferative neoplasms (MPNs) have somatic mutations that affect their pathogenesis, phenotype, and prognosis.
On 202 pretreatment MPN patient samples from the DALIAH trial and 135 samples collected after 24 months of therapy with recombinant interferon-alpha (IFNα) or hydroxyurea, targeted next-generation sequencing (NGS) was performed. Sequentially evaluating 120 genes with NGS made it possible to determine whether full clinicohematologic response (CHR) at 24 months and molecular response were related.
Patients with JAK2 mutations who received IFNα showed a larger decrease in the frequency of the JAK2 variant allele (median, 0.29 to 0.07; P<0.0001) when compared to those who did not (median, 0.27 to 0.14; P<0.0001). In contrast, neither in those who achieved CHR nor in those who did not do the CALR variant allele frequency markedly decreased. Patients treated with IFNα instead of hydroxyurea experienced more treatment-emergent changes in DNMT3A (P=0.04). Additionally, IFNα-treated patients who did not achieve CHR had a substantially higher prevalence of treatment-emergent DNMT3A mutations (P=0.02).
Age-adjusted odds ratio, 5.29; 95% confidence interval, 1.59-17.54; P=0.007; and a mutation in TET2 alone was significantly associated with previous stroke (age-adjusted odds ratio, 3.03; 95% confidence interval, 1.03-9.01; P=0.044). At 24 months, we discovered mutation-specific IFNα response patterns, including different molecular responses in JAK2- and CALR-mutated MPN and the emergence of DNMT3A-mutated clones/subclones in response to treatment.
Source:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC90062
Clinical Trial:https://clinicaltrials.gov/ct2/show/NCT01387763
Knudsen, T. A., Skov, V., Stevenson, K., Werner, L., Duke, W., Laurore, C., Gibson, C. J., Nag, A., Thorner, A. R., Wollison, B., Hansen, D. L., Ellervik, C., El Fassi, D., de Stricker, K., Ocias, L. F., Brabrand, M., Bjerrum, O. W., Overgaard, U. M., Frederiksen, M., Kristensen, T. K., Kruse, T.A., Thomassen, M., Mourits-Andersen, T., Severinsen, M.T., Stentoft, J., Starklint, J., Neuberg, D.S., Kjaer, L., Larsen, T.S., Hasselbalch, H.C., Lindsley, R.C., & Mullally, A. (2022). Genomic profiling of a randomized trial of interferon-α vs hydroxyurea in MPN reveals mutation-specific responses. Blood advances, 6(7), 2107–2119. https://doi.org/10.1182/bloodadvances.2021004856