KEY TAKEAWAYS
- A meta-analysis of seven phase-III and three phase-II trials compared the efficacy of immunotherapy versus placebo in patients with mCRPC.
- Immunotherapy, particularly ICBs, demonstrated a reduction in the likelihood of disease progression compared to placebo by 18%.
- No significant improvement in OS was observed with immunotherapy, but there was a significant increase in ORR among patients who underwent ICB therapy.
- No significant TRAEs were observed in association with the administration of immunotherapies, but ICBs resulted in a statistically significant increase in 3-4 grade TRAEs.
- The results were obtained from three phase-II clinical trials investigating the efficacy of ICBs in advanced prostate cancer, even in the absence of conventional therapies.
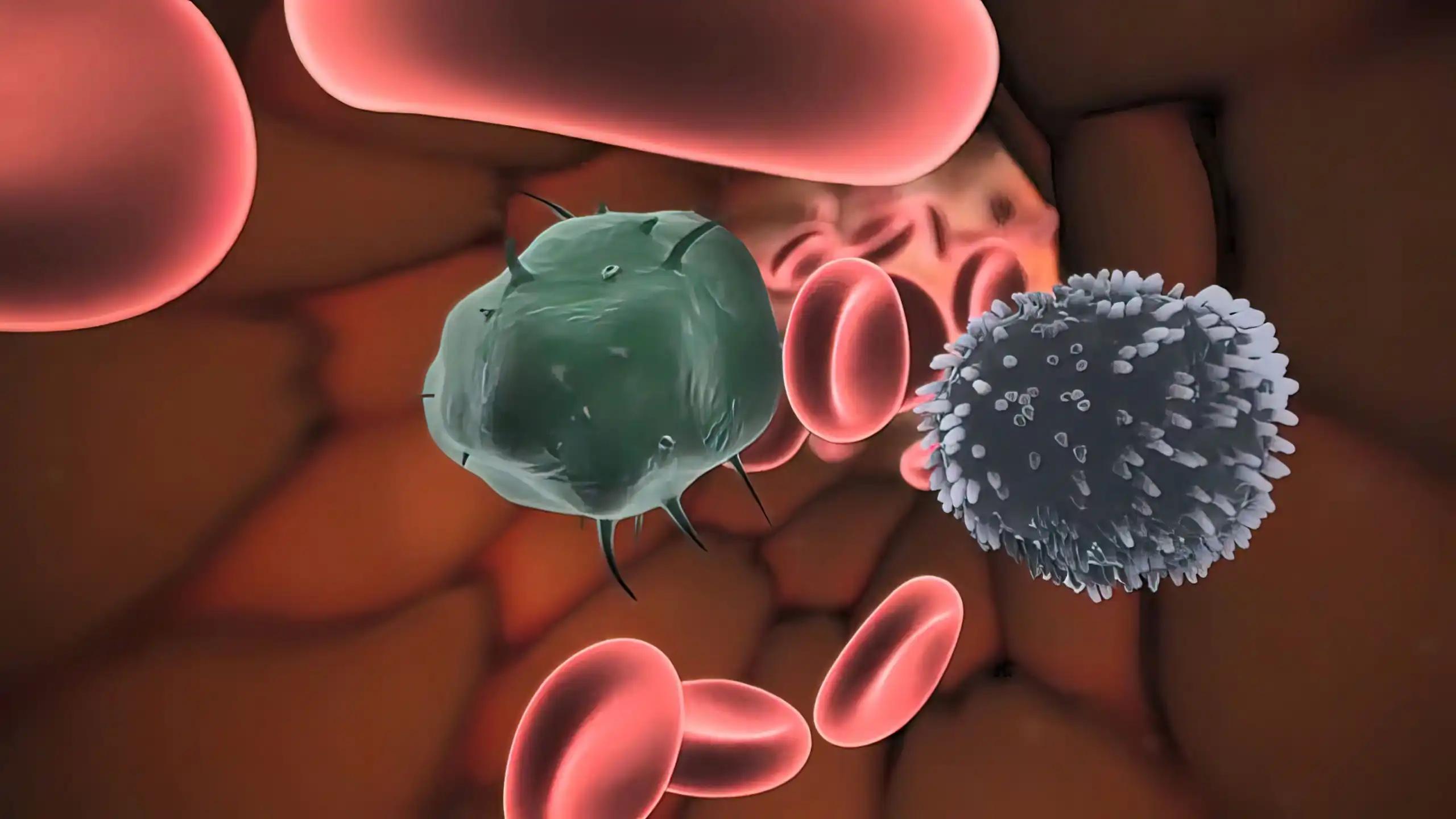
Immunotherapeutic interventions have surfaced as viable therapeutic options for managing metastatic castration-resistant prostate cancer (mCRPC). The efficacy and safety of immunotherapy in large-scale samples remain uncertain. A meta-analysis was conducted on seven phase-III randomized trials and three phase-II trials to compare the efficacy of immunotherapy versus placebo in patients with metastatic castration-resistant prostate cancer (mCRPC). The process of extracting data was carried out in accordance with the PRISMA statement. The assessed parameters included overall survival (OS), progression-free survival (PFS), overall response rate (ORR), and adverse events (AE). Three phase-II trials with results were identified based on the outcomes of randomized phase-III trials.
The overall survival (OS) of 4185 patients and progression-free survival (PFS) of 3320 patients were assessed. Compared to the placebo, the administration of immunotherapies did not significantly improve overall survival (hazard ratio = 0.90; 95% confidence interval 0.79-1.03; P = 0.13). Immunotherapies, particularly immune checkpoint inhibitors (ICBs), demonstrated a reduction in the likelihood of disease progression compared to placebo by 18% (hazard ratio = 0.82; 95% confidence interval 0.68-1.00; p = 0.04). The study revealed a noteworthy increase in objective response rate (ORR) among patients who underwent immune checkpoint blockade (ICB) therapy (RR = 1.90; 95%CI 1.30-2.78; P < 0.001). The administration of immunotherapies did not exhibit a significant association with any grade treatment-related adverse events (TRAEs) or 3-4 grade TRAEs, as evidenced by the odds ratios and corresponding 95% confidence intervals (OR = 1.01, 95% CI = 0.40-2.56; OR = 1.27, 95% CI = 0.72-2.25). Upon conducting subgroup analysis, it was observed that the use of ICBs resulted in a statistically significant increase in 3-4 grade TRAEs (OR = 2.85, 95% CI = 2.27-3.57), whereas the use of vaccines was associated with a statistically significant decrease in 3-4 grade TRAEs (OR = 0.78, 95% CI = 0.64-0.53). In addition, immune checkpoint inhibitors (ICBs) were found to elicit a favorable prostate-specific antigen (PSA) response [odds ratio (OR) = 2.43, 95% confidence interval (CI) 1.09-5.43, P = 0.03 (I2 = 0%, P = 0.83)].
These results were obtained from three phase-II clinical trials investigating the efficacy of ICBs in advanced prostate cancer, even in the absence of conventional therapies. Although immunotherapies do not have a significant impact on overall survival (OS), they do show notable improvements in progression-free survival (PFS) and objective response rate (ORR), particularly in the context of immune checkpoint blockade (ICB) treatment. No significant treatment-related adverse events (TRAEs) associated with administering immunotherapies were observed. On conducting a subgroup analysis, it was observed that immune checkpoint inhibitors (ICBs) and vaccines exhibited a noteworthy association with grade 3-4 treatment-related adverse events (TRAEs).
Source: https://pubmed.ncbi.nlm.nih.gov/36163285/
Clinical Trail: https://clinicaltrials.gov/ct2/show/NCT02111577
Zhang A, Tong D. Immunotherapy in patients with metastatic castration-resistant prostate cancer: a meta-analysis of data from 7 phase III studies and 3 phase II studies. Exp Hematol Oncol. 2022 Sep 26;11(1):63. doi 10.1186/s40164-022-00312-y. PMID: 36163285; PMCID: PMC9511714.