KEY TAKEAWAYS
- The phase 1 trial aimed to investigate the efficacy and safety of JNJ-75276617 in adult participants with R/R acute leukemia harboring KMT2A alterations.
- Researchers noticed encouraging antileukemic activity and an acceptable safety profile with JNJ-75276617 monotherapy in R/R acute leukemia harboring KMT2A or NPM1 alterations; additional information will be provided later.
Relapsed/refractory (R/R) acute leukemia with KMT2A (also called MLL1; 9-15% of adult acute myeloid leukemia (AML), 10% of Acute lymphoblastic leukemia(ALL)) or NPM1 (30% of adult AML) alterations often leads to poor outcomes. Menin-KMT2A interaction sustains leukemic cells with KMT2A and NPM1 alterations (Kuhn 2016), making it a target. JNJ-75276617, a potent inhibitor, shows promise in preclinical studies. This report presents initial data on JNJ-75276617 in adults with R/R acute leukemia harboring KMT2A alterations or NPM1 mutations.
Elias Jabbour and his team aimed to assess the ongoing dose escalation in 75276617ALE1001, with RP2D(s) yet to be determined.
The study analyzed ongoing Phase 1 clinical trial 75276617ALE1001 (NCT04811560), conducted at multiple centers. An open-label, multicenter trial focused on dose-finding for JNJ-75276617 in patients (pts) with R/R acute leukemia. Participants in dose escalation receive oral JNJ-75276617 on a 28-day cycle, exploring multiple dose levels (≥15 mg) with daily or twice-daily dosing as of 8 April 2023. Adverse events(AEs) were graded using CTCAE v5.0, and responses were assessed per ELN2017 criteria. Preliminary safety, efficacy, and pharmacodynamic (PD) data were reported, with a specific emphasis on efficacy in higher dose levels involving ≥3 dosed pts.
About 58 pts were administered JNJ-75276617, with a median age of 63 (range: 19-83) years; 56 pts (97%) had R/R AML, and 2 (3%) had R/R ALL. The median number of prior treatment lines was 2 (range: 1-7), including 10 (17%) with a prior allogeneic stem cell transplant (SCT). KMT2A or NPM1 alterations were present in 33 (57%) and 25 (43%) pts, respectively.
About 52% (30) of the pts experienced ≥1 treatment-related adverse event (TRAE), most commonly differentiation syndrome (DS) (8 [14%]), and in 17 (29%) pts had grade ≥3 TRAEs; those reported in ≥2 pts were neutropenia (6 [10%]), anemia and thrombocytopenia (4 [7%] each), DS (3 [5%]), and ALT and AST increase (2 [3%] each).. Notably, dose-limiting toxicities (DLTs) were observed in 5 (9%) pts, with DS (2 [3%]) as the only DLT reported in ≥2 pts.
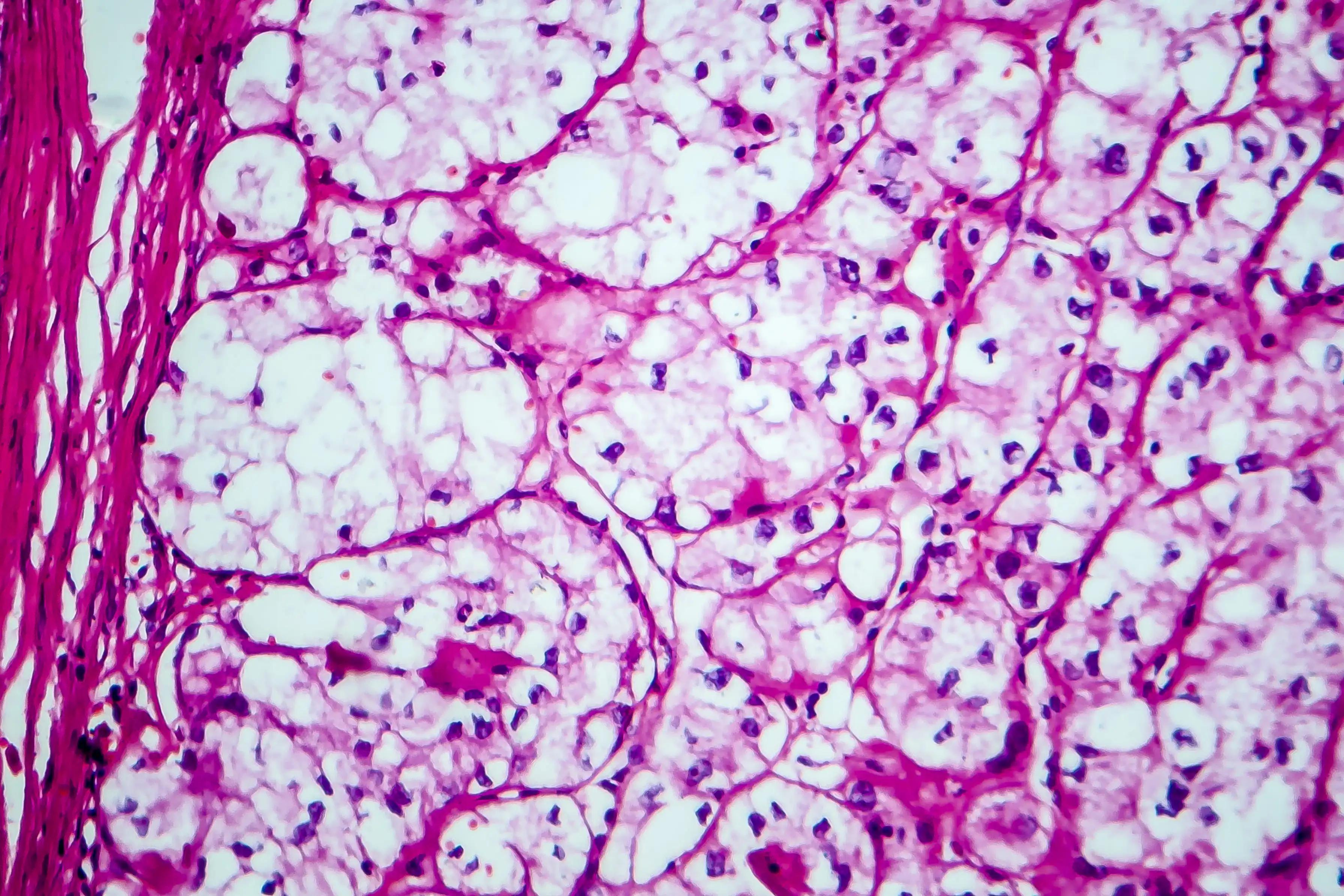
Among 41 pts with disease evaluation data, 26 (63%) showed a reduction in bone marrow (BM) disease burden, with a ≥50% decrease in BM blasts observed in 16 (39%) pts. In the highest dose level with ≥3 pts (90 mg BID; n=8), the overall response rate (ORR) (≥PR) was 50% (n=4), with all responders ongoing. These responders (2 NPM1-, 2 KMT2A-altered) achieved CR (1 pt), CRh (1 pt), and CRi (2 pts).
In a review of higher dose levels with ≥3 pts (≥45 mg BID; n=20), the ORR was 40% (n=8), with 7 responders ongoing. Responders (5 NPM1-, 3 KMT2A-altered) achieved CR (3 pts), CRh (1 pt), CRi (3 pts), and PR (1 pt); median (range) time to first response (≥PR) 1.81 mos (1.0-3.3; n=8); time to CR, CRh, or CRi 1.77 mos (1.0-3.3; n=7); and time to CR 2.79 mos (1.8-2.9; n=3).
Across all cohorts, 12 responders were identified, including 1 pts achieving minimal residual disease (MRD) negative CR. One responder discontinued treatment for allogeneic transplant, while 8 responders continue on treatment, including 2 pts in cycle 9.
Preliminary PD data from unfractionated BM and/or PBMCs in paired samples among responders (n=12) show biologic activity, indicated by a reduction in expression (mean fold change from baseline calculated as [on-tx-baseline]/baseline [range]) of menin-KMT2A target genes (MEIS1 -0.42 [-1.0-9.0]; HOXA9 -0.03 [-1.0-21.7]; FLT3 18.6 [-1.0-425]) and induction of genes associated with differentiation (ITGAM 55.0 [-0.93-1467]; MNDA 5.9 [-1.0-83.5]).
Compared to baseline, the percentage of KMT2A-altered cells, by break-apart FISH probe from 59.2% at baseline to 8.1% post-treatment and in NPM1 VAF using a myeloid gene NGS panel from 13.1% at baseline to 2.8% post-treatment.
The ongoing dose escalation in 75276617ALE1001 is yet to determine the recommended phase 2 dose(RP2D). Pts in the dose expansion phase will be administered JNJ-75276617 at the identified RP2D. Initial findings from this Phase 1 study indicate that JNJ-75276617 monotherapy exhibits a favorable safety profile, promising antileukemic activity, and emerging biologic effects aligning with the proposed mechanism of action in patients with R/R acute leukemia featuring KMT2A or NPM1 alterations.
The study is sponsored by Janssen Research & Development, LLC
Source: https://ash.confex.com/ash/2023/webprogram/Paper172422.html
Clinical Trial: https://clinicaltrials.gov/study/NCT04811560
Jabbour E, Searle E, Hay M A, et al. (2023).”A First-in-Human Phase 1 Study of the Menin-KMT2A (MLL1) Inhibitor JNJ-75276617 in Adult Patients with Relapsed/Refractory Acute Leukemia Harboring KMT2A or NPM1 Alterations.” Presented at ASH 2023 (Abstract 57).