KEY TAKEAWAYS
- Phase 2 trial acronym NADIM was conducted on patients with resectable stage IIIA (NSCLC).
- The study aimed to identify new biomarkers and mechanisms behind tumor responses to neoadjuvant chemoimmunotherapy and disease recurrence after surgery in patients with resectable stage IIIA NSCLC.
- Tumor bulk RNA sequencing was performed in 16 pretreatments and 36 post-treatment tissue samples from 41 patients with resectable stage IIIA NSCLC treated with neoadjuvant chemoimmunotherapy from the NADIM trial.
- The study found that CPR tumors had a stronger pre-established immune infiltrate at baseline than non-CPR and that a more significant effect of neoadjuvant therapy was seen in CPR tumors.
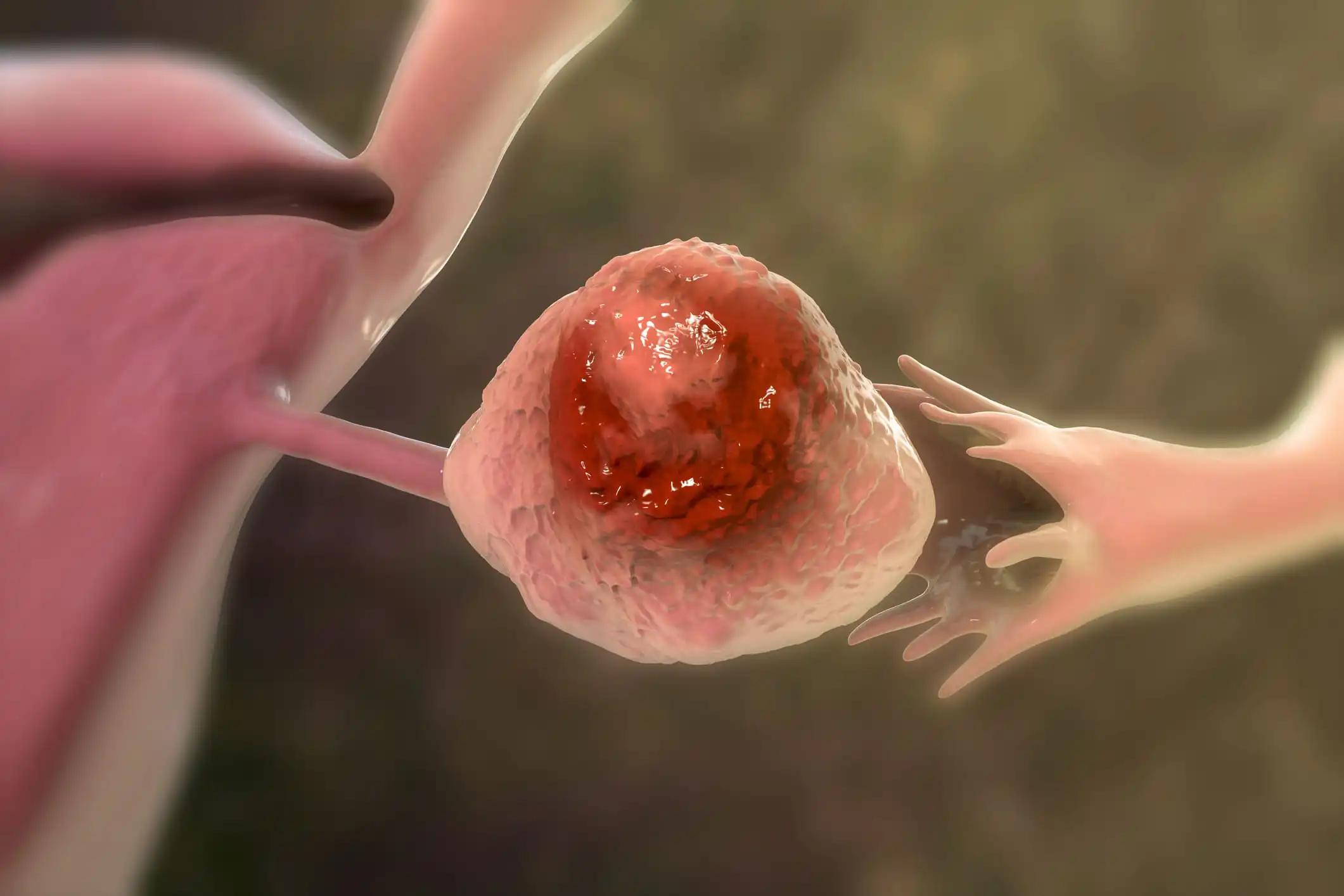
Since nivolumab plus chemotherapy for resectable stage IB-IIIA non-small cell lung cancer (NSCLC) (AJCC 7th edition) without ALK or EGFR alterations has improved pathological responses and survival rates compared with chemotherapy alone, it has been approved by the Food and Drug Administration (FDA). Unfortunately, many tumors do not respond adequately to treatment, which is linked to rapid disease advancement. The current state of knowledge prevents us from making such predictions. Researchers characterized this study’s gene expression profile of tumor samples to better understand tumor responses to neoadjuvant chemoimmunotherapy and disease recurrence after surgery. Forty-one patients with resectable stage IIIA NSCLC were treated with neoadjuvant chemoimmunotherapy in the NADIM trial. Tumor bulk RNA sequencing was performed on 16 samples taken before and 36 taken after treatment. Researchers used a panel that concentrated on 395 immune-related genes and pathways. The presence or absence of viable tumor cells in the tumor bed and lymph nodes examined during surgery determined whether a tumor had a complete pathological response (CPR). Pathway enrichment analysis and differentially expressed genes between groups were evaluated with DESeq2 and gene set enrichment analysis, respectively. Subtypes of immune cells were estimated in terms of their numbers using CIBERSORTx.
The area under the receiver operating characteristic curve (ROC) >0.9 for CPR prediction indicated that CPR tumors had a more robust pre-established immune infiltrate at baseline than non-CPR tumors, as evidenced by higher levels of IFNG, GZMB, NKG7, and M1 macrophages. Treatment with neoadjuvant therapy had a more significant impact on CPR tumors, as evidenced by a decrease in tumor markers and IFN signaling. In addition, higher dendritic cell and neutrophil proportions in post-treatment non-CPR samples were associated with relapse after surgery, as was higher expression of several genes, such as AKT1, BST2, OAS3, or CD8B. The post-treatment immune landscape, including the downregulation of proliferation markers and type I interferon signaling molecules in surgery samples, was also influenced by high PD-L1 and tumor mutational burden levels before treatment. The study findings provide further evidence of the distinction between CPR and non-CPR responses, describing potential immune mechanisms of response and relapse and providing hope for the individualization of immunotherapy-based regimens in the neoadjuvant setting of NSCLC.
Source: https://pubmed.ncbi.nlm.nih.gov/36171009/
Clinical Trial: https://clinicaltrials.gov/ct2/show/NCT03081689
Casarrubios M, Provencio M, Nadal E, Insa A, Del Rosario García-Campelo M, Lázaro-Quintela M, Dómine M, Majem M, Rodriguez-Abreu D, Martinez-Marti A, De Castro Carpeño J, Cobo M, López Vivanco G, Del Barco E, Bernabé R, Viñolas N, Barneto Aranda I, Massuti B, Sierra-Rodero B, Martinez-Toledo C, Fernández-Miranda I, Serna-Blanco R, Romero A, Calvo V, Cruz-Bermúdez A. Tumor microenvironment gene expression profiles associated to complete pathological response and disease progression in resectable NSCLC patients treated with neoadjuvant chemoimmunotherapy. J Immunother Cancer. 2022 Sep;10(9):e005320. doi: 10.1136/jitc-2022-005320. PMID: 36171009; PMCID: PMC9528578.