KEY TAKEAWAYS
- The EPIC trial aimed to present interim analysis of outcomes, patient characteristics, and treatment patterns in CLL post-acalabrutinib initiation.
- The interim analysis reported real-world acalabrutinib outcomes aligning with ELEVATE-TN trial findings, informing UK clinical decisions.
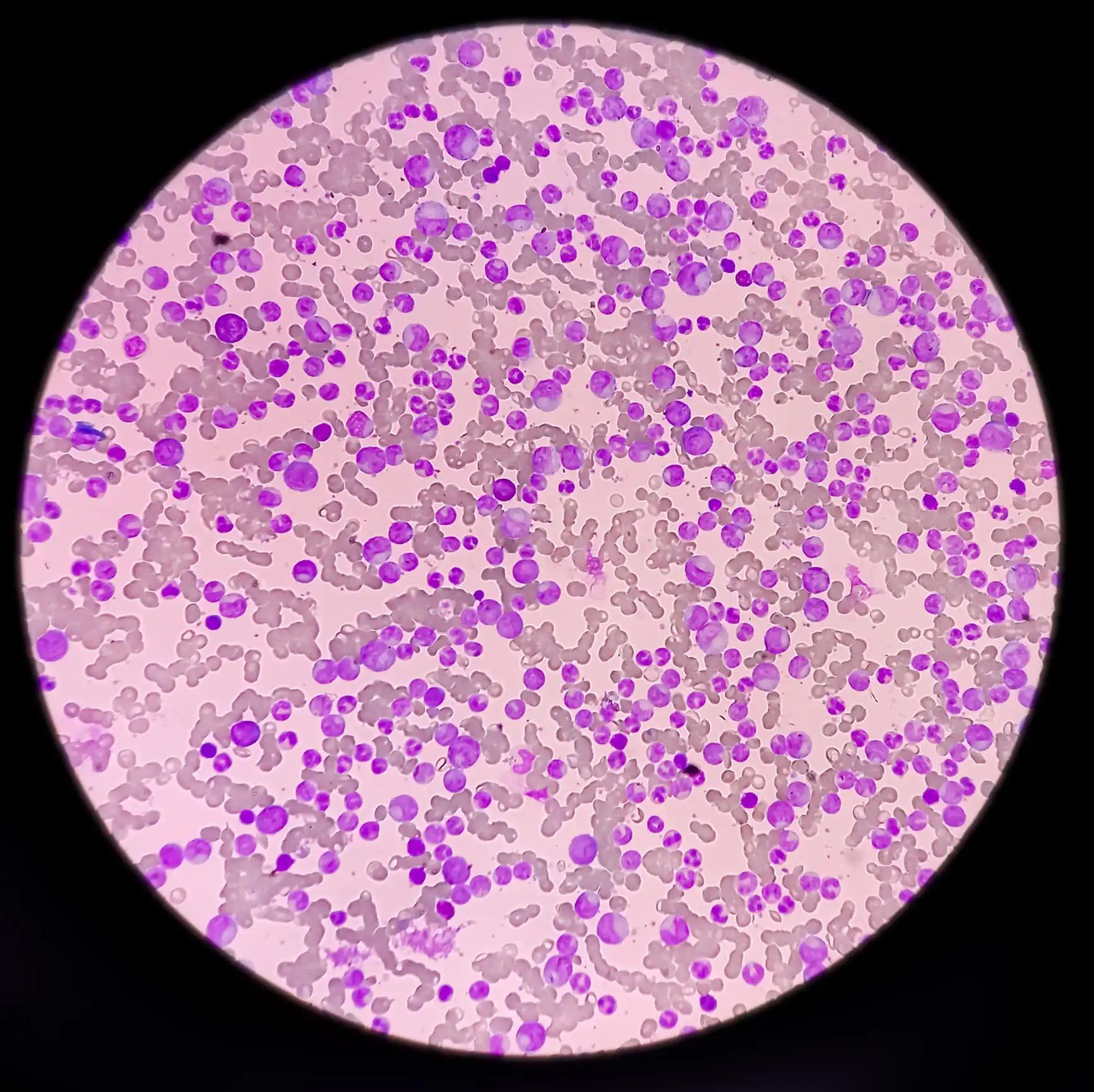
High response rates and acceptable safety profiles were noted in clinical trials of acalabrutinib, a second-generation Bruton’s tyrosine kinase inhibitor, for patients with chronic lymphocytic leukemia (CLL). Nonetheless, there is a scarcity of UK real-world data regarding the utilization of first-line acalabrutinib in patients with CLL.
Nicolas Martinez-Calle and the team aimed to deliver an interim analysis of outcomes, clinical features, and treatment trends in patients with CLL following the initiation of first-line acalabrutinib via the UK Early Access Programme (EAP), with a minimum follow-up of 24 months.
This retrospective multi-center cohort study, registered under ClinicalTrials.gov (NCT05557695), focused on patients with CLL eligible if treatment-naïve and beginning acalabrutinib via the EAP between April 1, 2020, and April 1, 2021.
Patients, recruited from 16 sites in England and Wales, were assessed for real-world progression-free survival (rwPFS), real-world overall survival (rwOS), and real-world overall response rate (rwORR) during first-line treatment.
Data included baseline clinical and demographic characteristics as well as acalabrutinib treatment patterns, sourced from medical records. The study intends to track patients for up to 60 months post-acalabrutinib initiation (index date), with a data cut-off on November 30, 2023.
The results revealed that this interim analysis comprised 170 patients, with a median age at index of 74.5 years (IQR, 68.3–79.6). Among them, 41% were female, and the majority were White British. Most patients had an Eastern Cooperative Oncology Group performance score of 0-1.
The median Cumulative Illness Rating Scale-Geriatric score at index was 4. Acalabrutinib was primarily administered at a dose of 100 mg bi-daily. The median duration of follow-up was 36.9 months. rwPFS rate at 12 and 24 months was 92.4% (95% CI, 88.4 – 96.4) and 87.0% (95% CI, 82.1 – 92.2), respectively. The rwOS rate at 12 and 24 months was 92.9% (95% CI, 89.2–96.9) and 88.2% (95% CI, 83.5–93.2), respectively. The rwORR at 12 and 24 months was 87.0% (95% CI, 80.6–93.7; n=101) and 86.0% (95% CI, 79.9–92.0; n=128), respectively.
At index, a notable proportion of patients had creatinine clearance <60 mL/min and various mutations were observed. The median time from CLL diagnosis to index was 3.2 years. A significant portion of patients had comorbidities such as hypertension, type-2 diabetes, kidney disease, and atrial fibrillation.
Treatment continuation rates at 12 and 24 months were 87.6% (95% CI, 82.7–92.7, n=169) and 79.3% (95% CI,73.4–85.6, n=169), respectively. At data cut-off, 24% (40/169) patients had discontinued acalabrutinib (1 had no record); 38% (15/40) of discontinuations were due to adverse events, 13% (5/40) disease progression, 5% (2/40) patients’ decision and 43% (17/40) other (1 patient had no reason recorded); most common adverse events leading to discontinuations (≥1 AE could be reported per discontinuation) included cardiovascular, haematoma, and Richter transformation (n=2 each).
The study concluded that real-world acalabrutinib outcomes, including a 24-month rwPFS rate of 87.0% and a treatment continuation rate of 79.3%, align with findings from the ELEVATE-TN trial (NCT02475681). These results offer valuable insights for clinical decision-makers regarding the utilization of acalabrutinib in UK settings.
The trial was sponsored by AstraZeneca.
Clinical Trial: https://clinicaltrials.gov/study/NCT05557695
Martinez-Calle N, Walewska R, Paneesha S, et al. (2024). “OUTCOMES OF EPIC: A NON-INTERVENTIONAL, OBSERVATIONAL STUDY OF PATIENTS WITH CHRONIC LYMPHOCYTIC LEUKAEMIA TREATED WITH FIRST-LINE ACALABRUTINIB VIA THE UK EARLY ACCESS PROGRAMME; INTERIM ANALYSES.” Presented at EHA 2024 (P1833).