KEY TAKEAWAYS
- The phase 3 trial aimed to investigate the efficacy of tisotumab vedotin as a 2- or 3L treatment in patients with recurrent cervical cancer.
- The primary end point was to determine OS.
- Researchers noticed significantly greater efficacy of tisotumab vedotin over chemotherapy in treating recurrent cervical cancer.
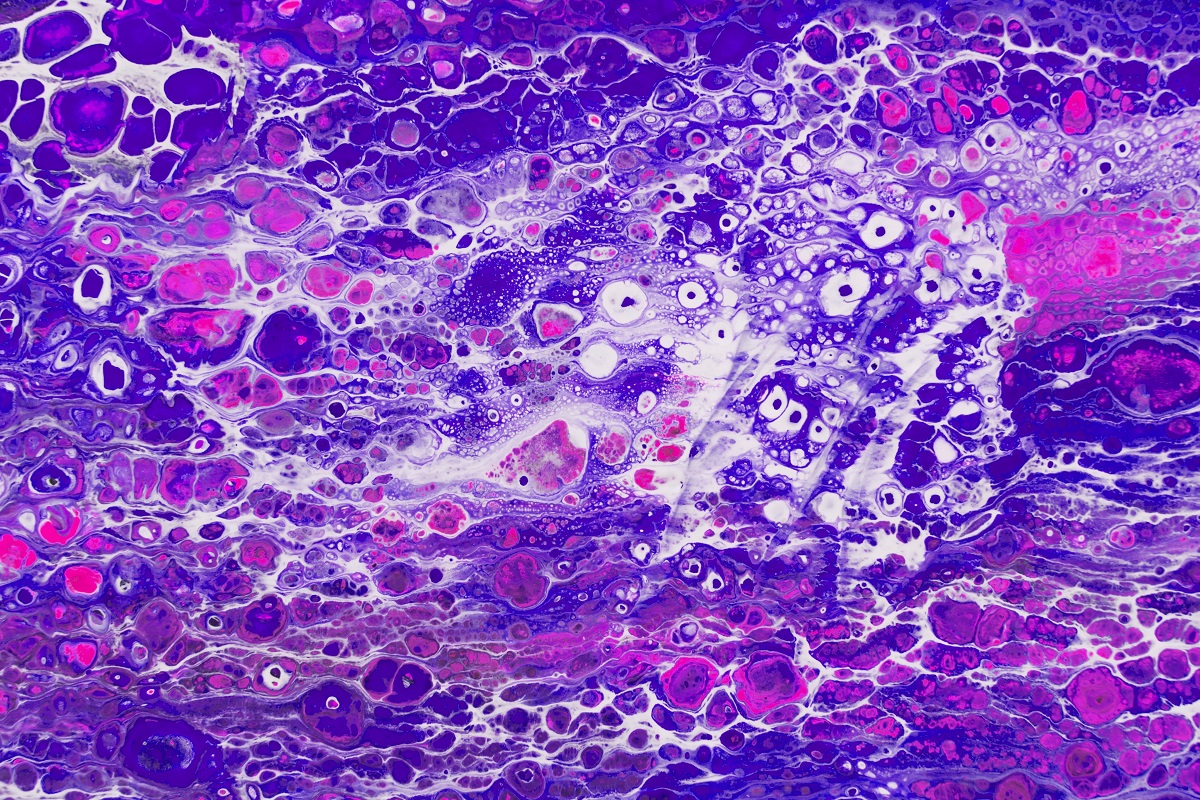
Recurrent cervical cancer is a life-threatening disease, with limited treatment options available when disease progression occurs after first-line (1L) combination therapy.
Ignace Vergote and the team aimed to focus on evaluating the effectiveness of tisotumab vedotin, an antibody-drug conjugate, as a second (2)- or third-line (3L) treatment option for patients with recurrent cervical cancer.
They performed an inclusive analysis through a phase 3, multinational, open-label trial to evaluate the efficacy of tisotumab vedotin as 2- or 3L therapy in patients with recurrent or metastatic cervical cancer. Patients were randomly assigned in a 1:1 ratio to receive either tisotumab vedotin monotherapy (2.0 mg per kilogram of body weight every 3 weeks) or the investigator’s choice of chemotherapy (topotecan, vinorelbine, gemcitabine, irinotecan, or pemetrexed). The primary endpoint of the study was overall survival (OS).
About 502 patients underwent randomization (253 were assigned to the tisotumab vedotin group and 249 to the chemotherapy group); the groups were similar with respect to demographic and disease characteristics. The median OS was significantly longer in the tisotumab vedotin group than in the chemotherapy group (11.5 months [95% CI, 9.8 to 14.9] vs. 9.5 months [95% CI, 7.9 to 10.7]), results that represented a 30% lower risk of death with tisotumab vedotin than with chemotherapy (HR, 0.70; 95% CI, 0.54 to 0.89; 2-sided P = 0.004).
The median progression-free survival (PFS) was 4.2 months (95% CI, 4.0 to 4.4) with tisotumab vedotin and 2.9 months (95% CI, 2.6 to 3.1) with chemotherapy (HR, 0.67; 95% CI, 0.54 to 0.82; 2-sided P<0.001).
The confirmed objective response rate (ORR) was 17.8% in the tisotumab vedotin group and 5.2% in the chemotherapy group (OR, 4.0; 95% CI, 2.1 to 7.6; 2-sided P<0.001). A total of 98.4% of patients in the tisotumab vedotin group and 99.2% in the chemotherapy group had at least 1 adverse event (AE) that occurred during the treatment period (defined as the period from day 1 of dose 1 until 30 days after the last dose); grade 3 or greater events occurred in 52.0% and 62.3%, respectively. A total of 14.8% of patients stopped tisotumab vedotin treatment because of toxic effects.
The study concluded that the analyzed adult AML population exhibited a higher frequency of BCR::ABL1 p190+ detection than reported in global literature. This underscores the necessity for further research to understand the underlying reasons for this higher incidence and to determine optimal treatment strategies.
The trial was sponsored by Seagen Inc.
Source: https://pubmed.ncbi.nlm.nih.gov/38959480/
Clinical Trial: https://clinicaltrials.gov/study/NCT04697628
Vergote I, González-Martín A, Fujiwara K, et al. (2024). “Tisotumab Vedotin as Second- or Third-Line Therapy for Recurrent Cervical Cancer.” N Engl J Med. 2024 Jul 4;391(1):44-55. doi: 10.1056/NEJMoa2313811. PMID: 38959480.