KEY TAKEAWAYS
- The KeyLargo phase II trial aimed to evaluate the efficacy of pembrolizumab in combination with oxaliplatin and capecitabine as a potential standard of care for first-line therapy for HER2-negative mEGC.
- NeXT Personal, a tumor-informed ctDNA assay, generated personalized liquid biopsy panels for MRD and CAV detection.
- The study found that Tumor-informed plasma-based ctDNA profiling in mEGC may detect known CAVs arising during therapy and inform therapeutic decisions.
Metastatic esophagogastric cancer (mEGC) is a deadly cancer of the stomach and esophagus with poor long-term survival. Studies have shown that combining anti-PD-1 therapy with chemotherapy is now the standard treatment for mEGC.
Researchers aimed to evaluate the efficacy of pembrolizumab in combination with oxaliplatin and capecitabine as a potential standard of care for first-line therapy for HER2-negative mEGC.
About 36 patients(pts) were enrolled in the study. Among the 34 pts for whom data could be evaluated, 25 exhibited a positive response to the treatment, resulting in an Overall Response Rate (ORR) of 74%. This response included 6 pts achieving a Complete Response (CR) and 19 pts experiencing a Partial Response (PR).
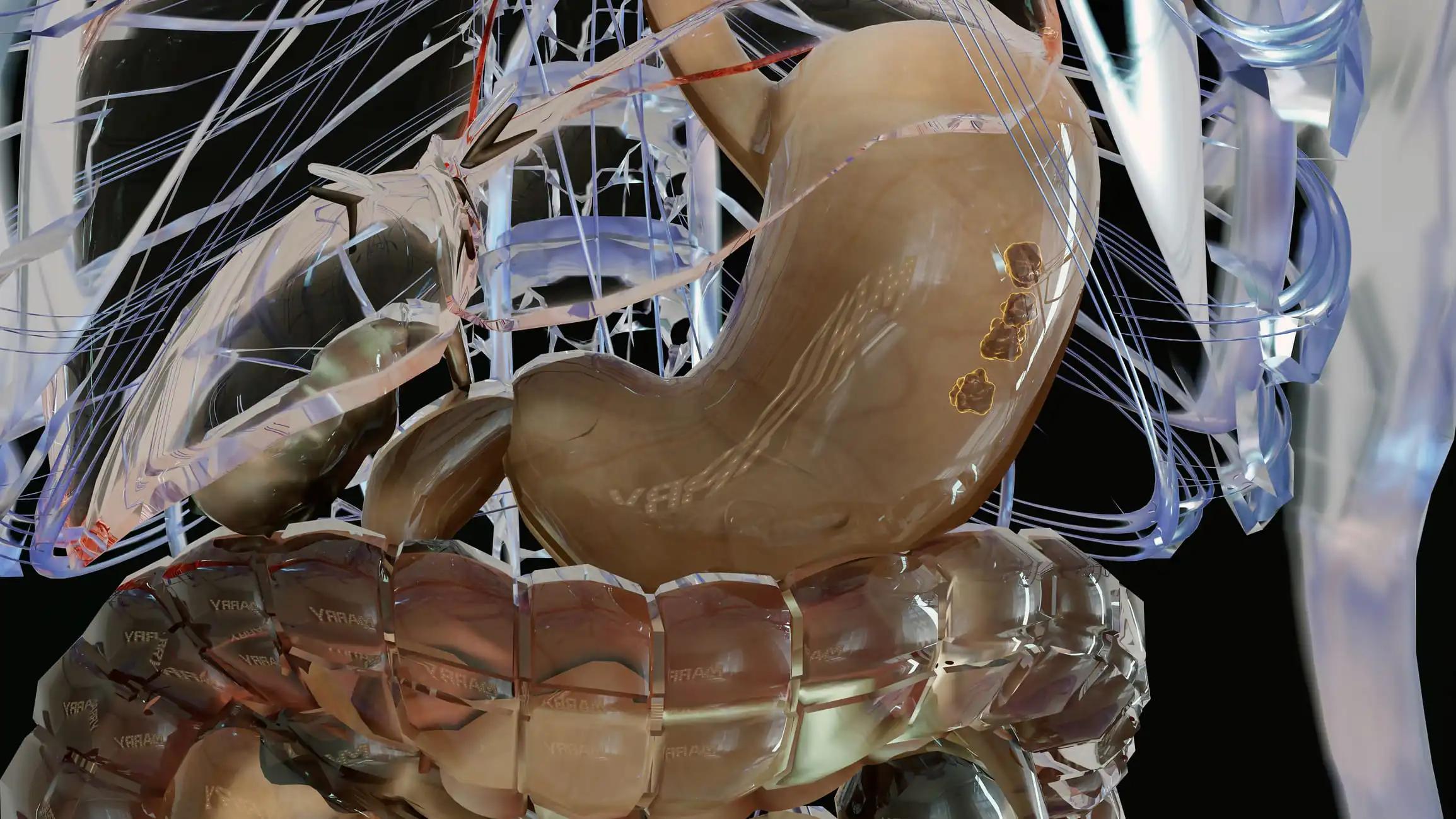
For the initial analysis, baseline tumor samples were collected from 16 pts, and 59 corresponding on-treatment (OT) plasma samples were taken up to cycle 35. A tumor-informed ctDNA assay known as NeXT Personal was employed. This assay generated personalized liquid biopsy panels using somatic variants (SV) identified through tumor whole genome sequencing. Each personalized assay incorporated up to 1,800 SVs, enhancing its sensitivity for minimal residual disease (MRD) detection. Additionally, it included a consistent set of 2,100 clinically actionable variants (CAV).
Of the 36 pts enrolled in the study, 32 had baseline tumor and longitudinal plasma samples collected and stored for testing. In the initial cohort of 16 pts, MRD events ranged from 5.3 to 302,000 parts per million (PPM). All 16 pts (100%) were MRD-positive at baseline, with a detection limit between 1.5 and 4.6 PPM. They collected OT samples every 3 cycles (9 weeks). The ratio of PPM (rPPM) between baseline and the first available OT sample (typically Cycle 4 to 7) correlated significantly with progression-free survival (PFS, P= 0.0004, logrank). rPPM was significantly reduced in pts achieving the best overall response of PR/CR (98% mean rPPM) compared to those with progressive disease (25% mean rPPM, P< 0.037, U-test). About 2 pts achieved complete remission(CR), each with 11/11 (100%) MRD-negative plasma samples over two years. They identified CAVs in longitudinal samples, with TP53 consistently detected in 5 pts, and a PIK3CA mutation emerged in the final 3 (of 9) time points from one patient.
The study found that Tumor-informed plasma-based ctDNA profiling in mEGC may detect known CAVs arising during therapy and inform therapeutic decisions.
Source: https://ascopubs.org/doi/abs/10.1200/JCO.2023.41.16_suppl.4040
Clinical Trial: https://clinicaltrials.gov/study/NCT03342937