KEY TAKEAWAYS
- ABBV-400, an ADC targeting c-Met with a potent Top1i payload, shows promising antitumor activity in preclinical models and is undergoing a first-in-human study for NSCLC, GEA, and CRC treatment.
- The primary endpoints were safety, tolerability, PK, recommended phase 2 dose, and preliminary efficacy. The secondary endpoints were PK, safety, and preliminary efficacy.
- Clinical activity was observed with ABBV-400, with an ORR of 24.4%. PRs were also observed in patients with NSCLC, uterine cancer, and acral melanoma.
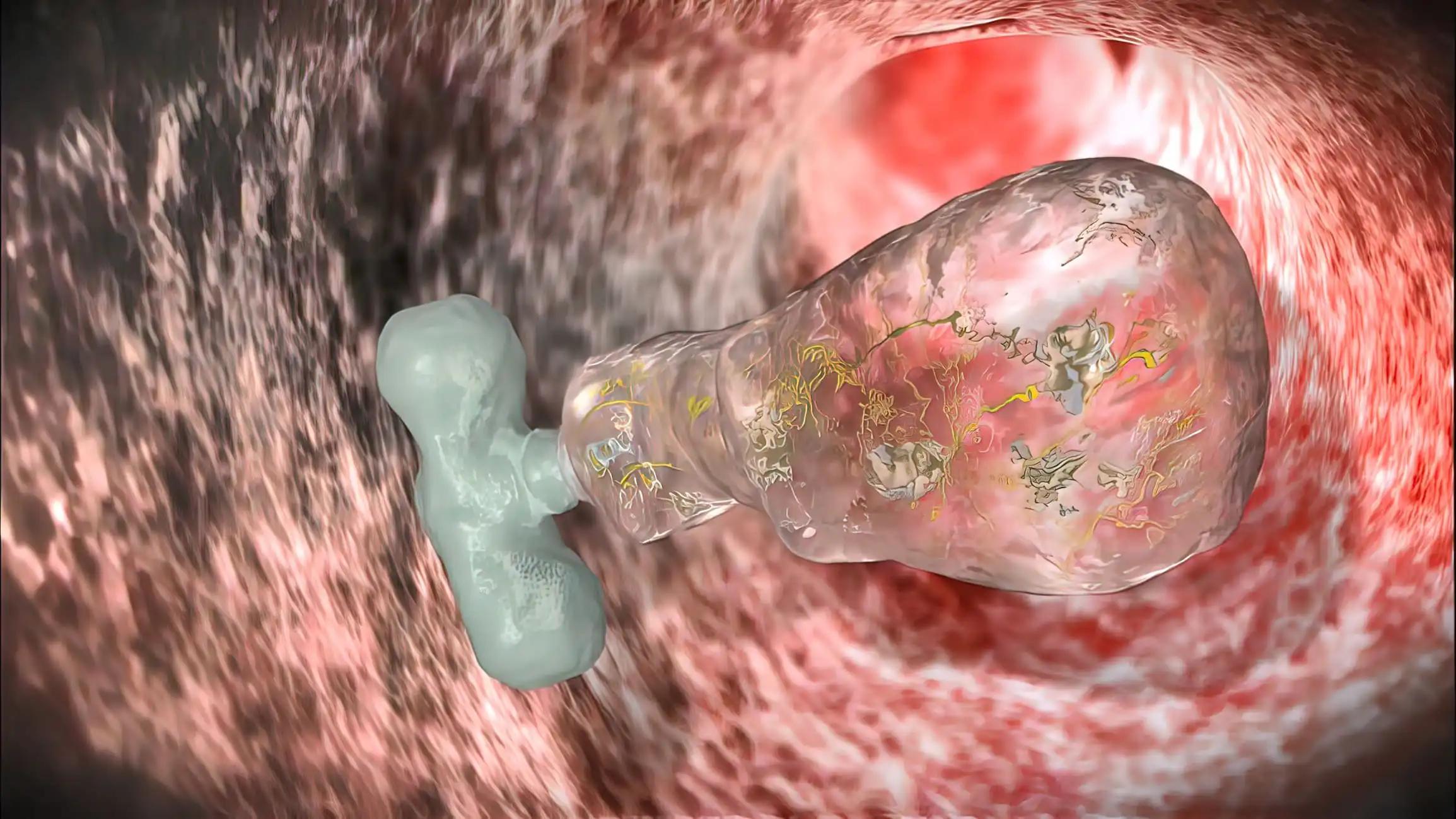
Non-small cell lung cancer (NSCLC), gastroesophageal adenocarcinoma (GEA), and colorectal cancer (CRC) are characterized by a high frequency of c-Met overexpression. C-Met overexpression is a potential therapeutic target as no existing treatments target it.ABBV-400, an antibody-drug conjugate (ADC), addresses this unmet need by combining the c-Met–targeting antibody telisotuzumab with a potent topoisomerase 1 inhibitor (Top1i) payload. ABBV-400 shows sustained antitumor activity in preclinical c-Met-expressing NSCLC, GEA, and CRC models. The study explored the dose escalation of the first-in-human study of ABBV-400 monotherapy.
This study, initiated by patients with advanced solid tumors, involved a phase 1 dose-escalation/expansion of ABBV-400. The primary goals were to assess the safety, tolerability, and pharmacokinetics (PK) of ABBV-400, establish the recommended phase 2 dose, and evaluate preliminary efficacy. PK characterization included the conjugate, total antibody, and free payload. During dose escalation, adults (≥18 years) with developed solid tumors that had advanced on standard treatments were enrolled with no restrictions based on c-Met overexpression status.
A total of 47 patients were enrolled in the study’s dose escalation phase (January 2023), with a median follow-up of 6.5 months. Median age was 58 years (34–79); 25 (53%) were male. Common cancers included CRC (n=21), NSCLC (n=5), and GEA (n=5). Median prior treatment lines were 4 (1–13). Hematologic adverse events included anemia (66%; G≥3: 38%), neutropenia (62%; G≥3: 43%), thrombocytopenia (43%; G≥3: 26%), and leukopenia (32%; G≥3: 19%). Non-hematologic AEs were nausea (60%, all grades 1–2), fatigue (49%; G≥3: 4%), and vomiting (38%, all grades 1–2). One of the patients was diagnosed with grade 1 interstitial lung disease.
Neutropenia and thrombocytopenia were dose-limiting toxicities (DLTs), dose and exposure-dependent. ABBV-400 showed clinical activity with an objective response rate of 24.4% (11/45; 95% CI: 12.9, 39.5). All responses were confirmed partial responses (PR). Additionally, 23 patients (50.0%) had stable disease (SD), and 7 (15.2%) had progressive disease. In CRC patients, 4/21 (19.0%) had a PR, and 13/21 (61.9%) had durable SD, with a disease control rate of 81.0% (95% CI: 58.1, 94.6). Outside CRC, PRs were seen in NSCLC (EGFR wildtype and mutant), uterine cancer, and acral melanoma.
A tolerable dose of ABBV-400 was identified and showed promising antitumor activity, supporting further evaluation in NSCLC, GEA, and CRC.
Source: https://ascopubs.org/doi/10.1200/JCO.2023.41.16_suppl.3015
Clinical Trial: https://www.clinicaltrials.gov/study/NCT05029882
Manish Sharma, Yasutoshi Kuboki, D. Ross Camidge, Ruth Perets, David Sommerhalder, Noboru Yamamoto, Jair Bar, Apurvasena Parikh, Rui Li, Gladys Morrison Thiele, Martha Raluca Neagu Aristide, Kevin Jay Freise, John D. Powderly. DOI 10.1200/JCO.2023.41.16_suppl.3015, J Clin Oncol 41, 2023 (suppl 16; abstr 3015).