KEY TAKEAWAYS
- The phase 2 trial aimed to investigate the efficacy of FOLFOX followed by short-course radiation in achieving a cCR for potential NOM in LARC patients.
- The primary endpoint was to determine the rate of cCR,
- Researchers observed promising local control with FOLFOX and SCRT in LARC patients.
The emerging standard of care (SOC) for locally advanced rectal cancer (LARC) is total neoadjuvant therapy (TnT). Limited prospective studies have focused on chemotherapy and short-course radiation (SCRT) to achieve complete clinical response (cCR) for potential non-operative management (NOM).
Janice Zhao and the research team aimed to assess the efficacy of the TnT approach as a novel SOC for LARC.
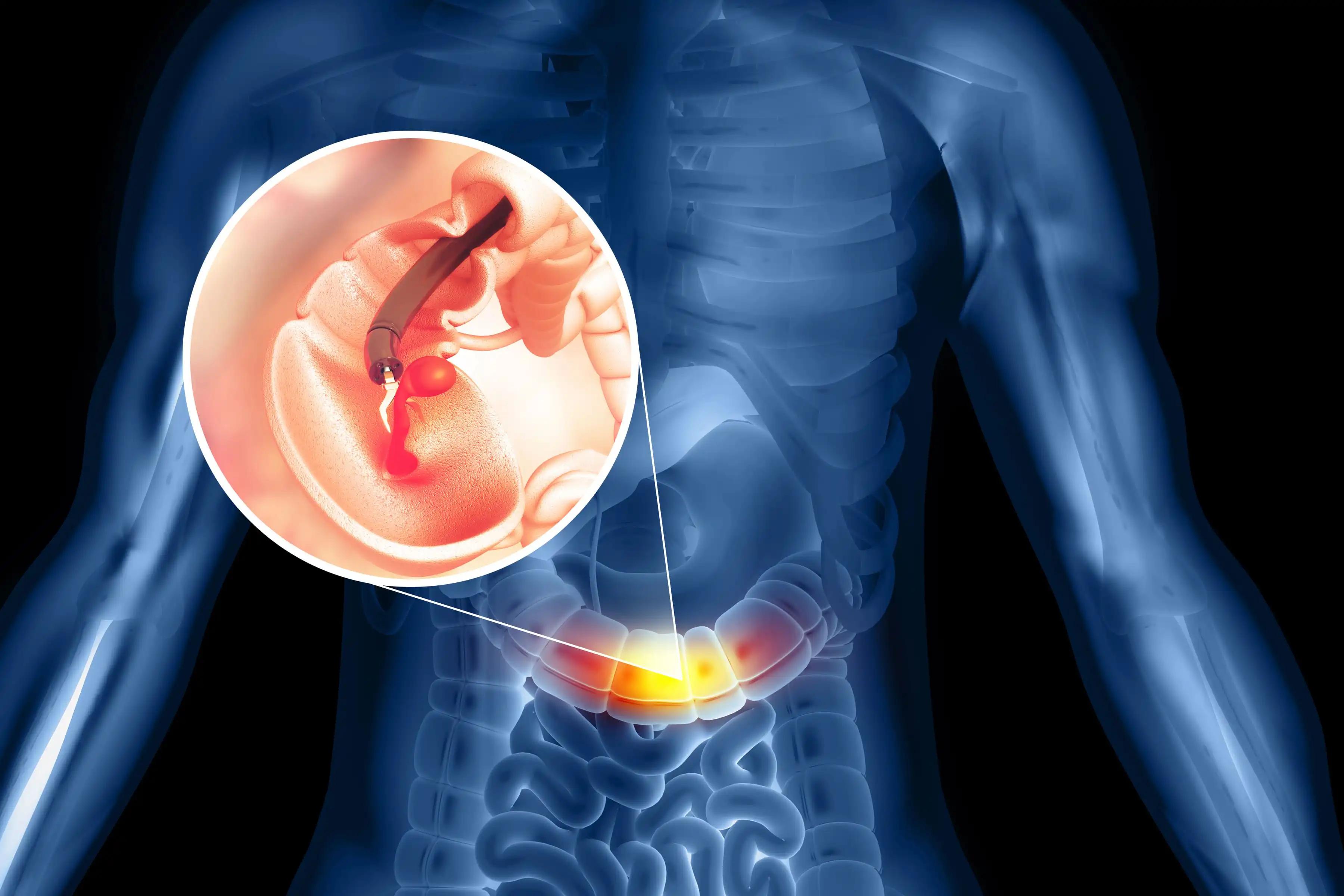
They conducted an inclusive analysis involving treatment-naïve adults with non-metastatic clinical T2-3N0 or T1-3 with N1-2a rectal adenocarcinoma in an open-label, single-arm clinical trial. Excluding patients requiring abdominoperineal resection for low rectal tumors, the trial assessed TnT comprising 5-fluorouracil, leucovorin, and oxaliplatin (mFOLFOX6) administered every 2 weeks for 10-12 cycles, followed by Short Course Radiation Therapy (SCRT). SCRT involved 25 Gy in 5 fractions to the rectal tumor and 20 Gy in 5 fractions to lymph node regions.
The primary endpoint was the rate of cCR, defined as a normal digital rectal exam (DRE) and endoscopic evaluation with normal mucosa or scar appearing without nodularity or ulcerations. Near complete response (nCR) was defined as DRE with smooth or minor mucosal abnormalities and endoscopic exam with superficial ulceration or erythematous scar. Patients achieving cCR or nCR after TnT were offered NOM with close surveillance, while others underwent Total Mesorectal Excision (TME). Secondary endpoints included 1-year disease-free survival (DFS) from the time of cCR (for NOM) or time of TME, overall survival (OS), and the R0 surgical resection rate.
About 12 patients, with a mean age of 51.4 years (7 males), enrolled in the study. The mean distance of the primary tumor from the anal verge was 9.7 cm. The median follow-up duration was 3.1 years. 25% (3 out of 12) achieved cCR, and 1 patient achieved nCR. All 4 patients with at least nCR underwent NOM according to the protocol. The patient with nCR experienced local regrowth and subsequently underwent TME. However, all 3 patients with cCR remained free of disease on NOM.
For secondary outcomes, the 1-year DFS was 100%. The Median OS was not reached at the time of analysis. Unfortunately, one patient had died; this patient, initially believed to have benign lung nodules at enrollment, was later diagnosed with metastatic disease. All surgical resections were R0, and no local recurrence occurred after TME. The study was prematurely closed following the OPRA trial results publication, which demonstrated the benefits of initiating radiation first in the TnT sequencing.
The study concluded that TnT with FOLFOX followed by SCRT demonstrates potential validity in treating LARC. Notably, excellent local control was observed with no local recurrence after TME. However, with only 25% of patients remaining on NOM and a lower NOM offering (33%) compared to the OPRA trial (74%), the findings suggest that this approach may not be optimal for organ preservation as the primary treatment goal in LARC.
The study is sponsored by University of Rochester
Source: https://meetings.asco.org/abstracts-presentations/229096
Clinical Trial: https://clinicaltrials.gov/study/NCT03781323
Zhao J, Gim G, Baran A M, et. al(2024). “Total neoadjuvant therapy (TnT) with FOLFOX followed by short course radiation in locally advanced rectal cancer: A phase II study.” Presented at ASCO-GI 2024 (Abstract 122).