KEY TAKEAWAYS
- The phase 3 ANCHOR trial examined whether treating anal HSIL reduces the incidence of anal cancer in HIV-positive patients.
- The study compared the incidence of anal cancer in HIV-positive persons treated for anal HSIL versus those under active monitoring without treatment.
- HIV-positive adults 35 years or older with biopsy-proven anal HSIL were included. HSIL therapy or active monitoring without treatment was randomly allocated.
- Treatment possibilities were for office-based ablation, anaesthesia-induced ablation or excision, topical fluorouracil, or imiquimod.
- Time-to-event analysis showed anal cancer incidence. Both groups had high-resolution anoscopy and biopsy for HSIL or malignancy.
- Treatment for anal HSIL reduced the rate of progression to anal cancer by 57% compared to active monitoring without therapy.
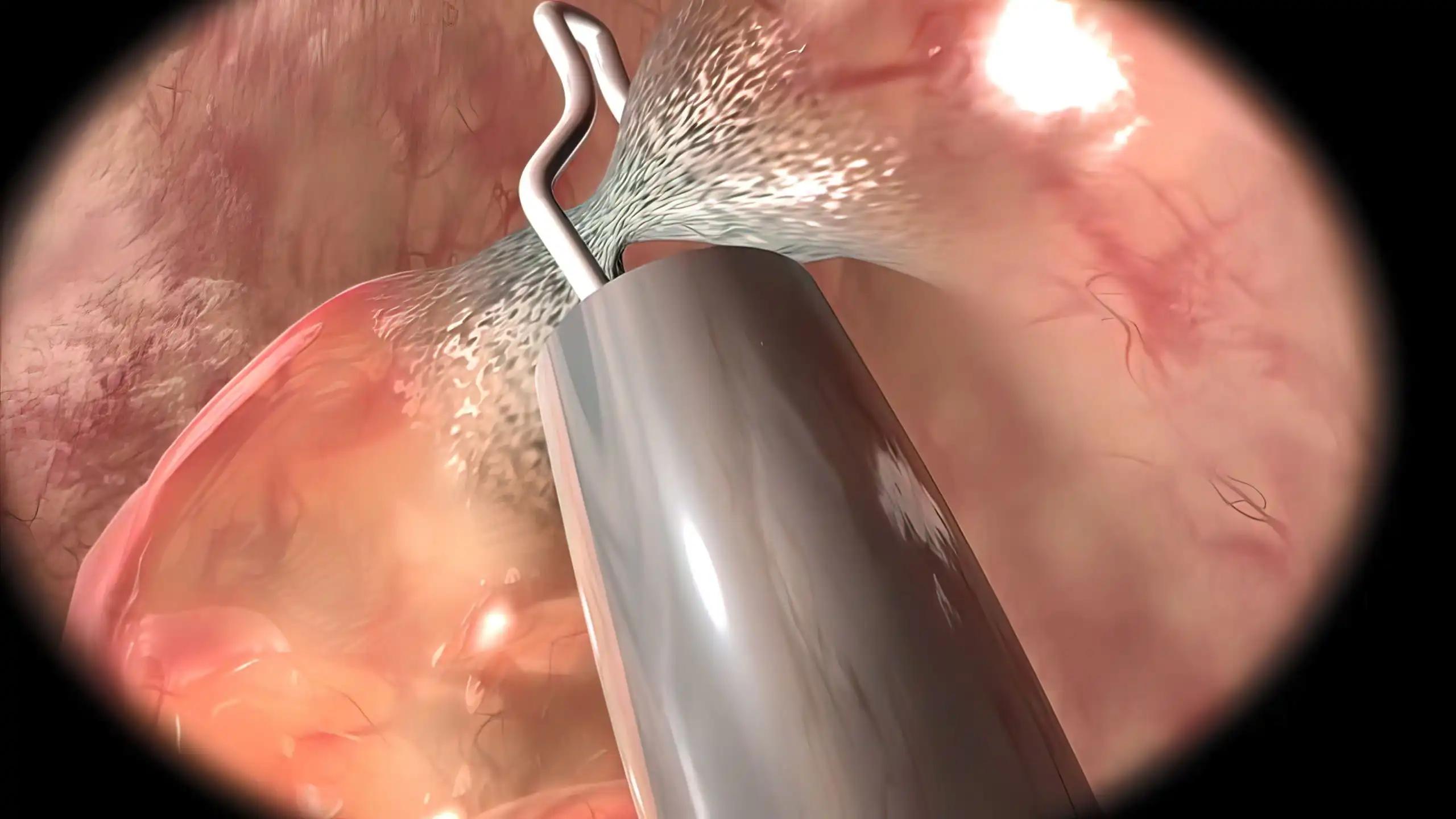
Those infected with human immunodeficiency virus (HIV) have a significantly higher risk of developing anal cancer than the average population. High-grade squamous intraepithelial lesions, also seen in the cervical epithelium, are a precursor to anal cancer. Therapy for cervical HSIL decreases the likelihood of cervical cancer developing, but there is a lack of information from prospective studies on the effectiveness of treating HSIL to prevent anal cancer. Researchers have 25 locations across the United States participating in their phase 3 experiment. HSIL treatment or active monitoring without treatment was randomly assigned to HIV-positive individuals aged 35 and up with biopsy-proven anal HSIL. Treatment methods included surgical excision, ablation, topical fluorouracil, or imiquimod administered at a doctor’s office. Anal cancer progression was the primary endpoint in the time-to-event analysis. Patients in the treatment group continued to receive medication until their HSIL symptoms subsided entirely.
High-resolution anoscopy was performed at least every 6 months in both groups, and biopsies were taken when necessary due to concerns about cancer or when persistent HSIL was detected in the therapy group and once a year in the active-monitoring group. A total of 4459 people were randomized, and 4446 of them (99.7%) were included in examining the time to cancer development. 9 instances were reported in the therapy group (173 per 100,000 person-years; 95% CI, 90 to 332), and 21 cases were diagnosed in the active-monitoring group (402 per 100,000 person-years; 95% CI, 262 to 616), with a median follow-up of 25.8 months. The therapy group had a 57% (95% CI, 6 to 80) reduced rate of development to anal cancer than the active-monitoring group (P = 0.03 by log-rank test). Treatment for anal HSIL reduced the risk of anal cancer among patients with biopsy confirmation compared to active monitoring.
Source: https://pubmed.ncbi.nlm.nih.gov/35704479/
Clinical Trail: https://clinicaltrials.gov/ct2/show/NCT02135419
Palefsky JM, Lee JY, Jay N, Goldstone SE, Darragh TM, Dunlevy HA, Rosa-Cunha I, Arons A, Pugliese JC, Vena D, Sparano JA, Wilkin TJ, Bucher G, Stier EA, Tirado Gomez M, Flowers L, Barroso LF, Mitsuyasu RT, Lensing SY, Logan J, Aboulafia DM, Schouten JT, de la Ossa J, Levine R, Korman JD, Hagensee M, Atkinson TM, Einstein MH, Cracchiolo BM, Wiley D, Ellsworth GB, Brickman C, Berry-Lawhorn JM; ANCHOR Investigators Group. Treatment of Anal High-Grade Squamous Intraepithelial Lesions to Prevent Anal Cancer. N Engl J Med. 2022 Jun 16;386(24):2273-2282. doi: 10.1056/NEJMoa2201048. PMID: 35704479; PMCID: PMC9717677.