KEY TAKEAWAYS
- The study aimed to investigate the immunomodulatory effects of entinostat on the TME of PDA.
- The primary endpoint was to determine ORR.
- Researchers noticed that entinostat and nivolumab promise to improve outcomes in patients with PDA; further investigation is ongoing.
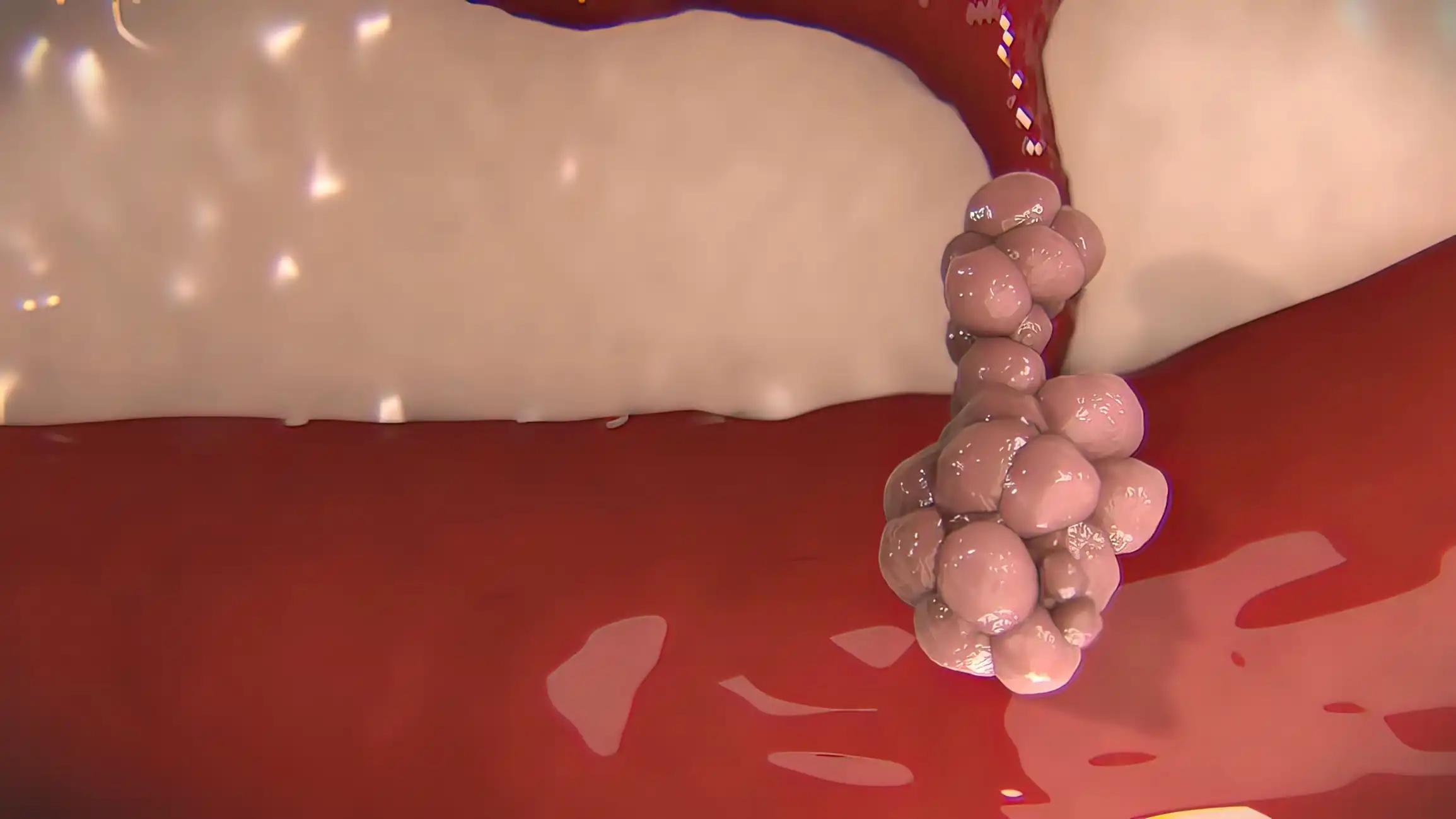
The tumor microenvironment (TME) of pancreatic ductal adenocarcinoma (PDA) is characterized by a paucity of cytotoxic tumor-infiltrating lymphocytes, an abundance of immune-suppressive cell populations, and a general resistance to immune checkpoint inhibitor (ICI) therapy. In preclinical models of PDA, the HDAC inhibitor entinostat modulated the transcriptional programming of myeloid cells, reducing their capacity for immunosuppression and sensitizing tumors to ICI therapy.
M. Baretti and the team aimed to assess the immunomodulatory effects of entinostat on the TME of PDA.
Researchers performed an inclusive analysis of a single-center, open-label, Simon two-stage, phase II study of entinostat in combination with the PD1 inhibitor nivolumab in patients with advanced PDA. Patients received oral entinostat 5 mg once a week, followed by concurrent entinostat 5 mg orally once a week plus nivolumab 240 mg intravenously every 2 weeks after a 14-day lead-in with entinostat monotherapy. Therapy continued with entinostat 5 mg weekly plus nivolumab at a dose of 480 mg fixed dose every 4 weeks until progression or unacceptable toxicities.
The primary endpoint was the objective response rate (ORR) by RECIST version 1.1. Peripheral immune profiles were assessed by high-dimensional mass cytometry by time of flight (CyTOF) and by Luminex of chemokines in the plasma. Changes in the TME were evaluated on the paired baseline and treatment biopsies by multiplexed immunohistochemistry (mIHC), image cytometry-based quantification, and bulk RNA-seq analysis.
About 27 evaluable patients were enrolled from November 2017 to November 2020. Three patients achieved a partial response (PR) by RECIST v1.1 criteria, resulting in an ORR of 11% (95% CI, 0.024-0.292), with a median response duration of 10.2 months.
Grade ≥3 treatment-related adverse events (TRAEs) were observed in 19 (63%) patients, with the most common being decreased lymphocyte count, anemia, hypoalbuminemia, and hyponatremia.
Entinostat treatment increased dendritic cell (DC) activation, maturation, migration, antigen processing, and presentation in the periphery, indicating HDAC inhibitor-mediated myeloid reprogramming. Gene expression analysis of paired baseline and on-treatment tumors enriched inflammatory response signaling pathways with combination treatment.
The study concluded that entinostat and nivolumab exhibited durable radiological responses in a subset of patients with PDA. Paired tissue and peripheral analysis revealed immunomodulation of myeloid cell populations, aligning with the preclinical hypothesis.
This research establishes a roadmap for future combinatorial therapeutic approaches to enhance PDA patients’ clinical benefits further.
The trial was sponsored by the Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins.
Source: https://www.abstractsonline.com/pp8/#!/20272/presentation/11431
Clinical Trial: https://clinicaltrials.gov/study/NCT03250273
Baretti M., Danilova L., Durham J. N., et al. (2024). “Immunomodulation of the tumor microenvironment of pancreatic ductal adenocarcinoma with histone deacetylase inhibition: Results of a phase 2 clinical trial of entinostat in combination with nivolumab.” Presented at AACR 2024 (Abstract CT016).