KEY TAKEAWAYS
- The phase II study investigated if the microbiome could be a predictive factor in identifying mCRC patients to benefit from ICI.
- This analysis suggested that SGBs can be a valuable biomarker for predicting atezo’s effects in pMMR mCRC patients.
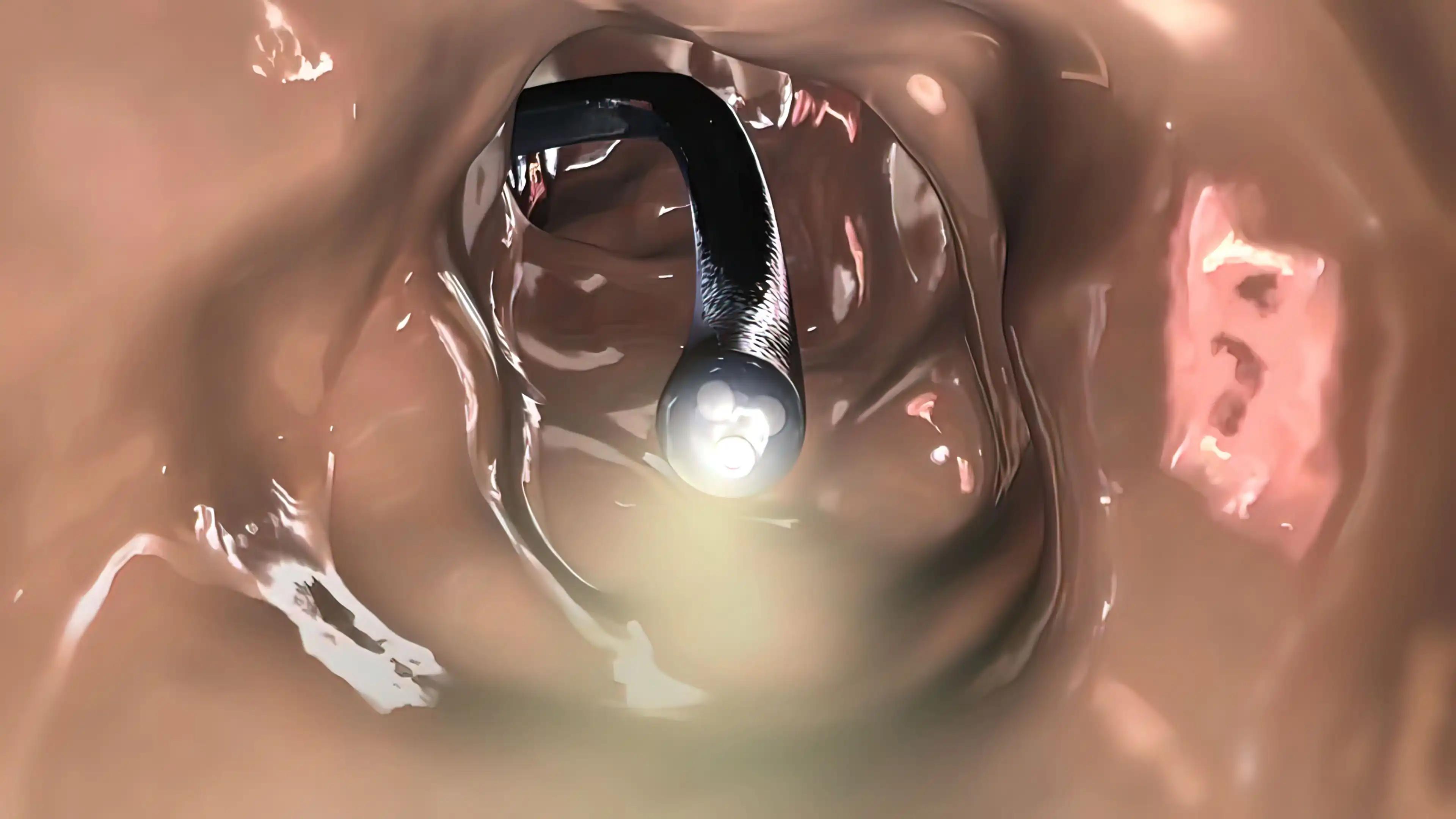
The gut microbiome is a potential marker of clinical benefit with immune checkpoint inhibitors (ICIs), but no data is currently available for metastatic colorectal cancer (mCRC). The AtezoTRIBE study, which explored the impact of adding atezolizumab (atezo) to FOLFOXIRI plus bevacizumab (bev) as a first-line treatment for mCRC, demonstrated an extension in progression-free survival (PFS). However, this benefit was observed to be limited for patients (pts) with proficient mismatch repair (pMMR) tumors. This study investigated whether the microbiome could serve as a predictive factor for identifying mCRC pts who could derive benefit from ICI treatment.
The AtezoTRIBE trial was a phase II study involving 218 mCRC pts, with no specific selection based on MMR status. Patients were randomly assigned in a 1:2 ratio to receive either first-line FOLFOXIRI/bev (arm A) or FOLFOXIRI/bev/atezo (arm B). Stool samples were collected prospectively. Researchers analyzed metagenomic (MG) data obtained from whole genome sequencing (WGS) at the level of species genome bins (SGBs). These analyses were adjusted for clinical and tumor-related factors and fold-ratios. Patients who experienced a PFS of 12 months or longer were categorized as responders (R).
Stool samples were initially obtained from 171 pts (78% of the total, with 55 in arm A and 116 in arm B), but only 163 samples were usable for metagenomic (MG) analysis. Among these pts, those with deficient MMR (dMMR) tumors (N=10) exhibited significantly lower MG diversity compared to those with proficient MMR (pMMR) tumors (N=148). The latter group had oral bacteria and pathobionts in their microbiomes, although the inherent immunogenicity of these microorganisms had not been confirmed.
For pMMR mCRC pts, the baseline composition of the microbiome did not show significant differences between the treatment arms. While microbiome diversity did not significantly differ between responders (R) and non-responders (not-R) in both arms, specific immunogenic SGBs (members of the Lachnospiraceae family) were more prevalent in responders treated in arm B. Veillonellaceae, and pathobionts were associated with a poor prognosis and/or variations in the benefit from the addition of atezo. At the same time, Fusobacterium nucleatum was linked to a poor prognosis, particularly in arm B.
This study represented the most extensive prospective examination indicating that SGBs could serve as a valuable biomarker for predicting the potential positive or negative impact of atezo in pMMR mCRC pts. The study’s findings suggested the need to develop microbiota-focused diagnostic tests to identify pMMR mCRC pts more likely to gain advantages from ICI-based treatment strategies.
Source: https://www.annalsofoncology.org/article/S0923-7534(23)00636-1/fulltext
Clinical Trial: https://classic.clinicaltrials.gov/ct2/show/NCT03721653
Marmorino, F., Piccinno, G., Rossini, D., Ghelardi, F., Murgioni, S., Salvatore, L., Nasca, V., Antoniotti, C., Daniel, F., Schietroma, F., Conca, V., Costa Silva, C.A., Tamburini, E., Tamberi, S., Passardi, A., Carullo, M., Antonuzzo, L., D’Onofrio, R., Zitvogel, L., Cremolini, C., Derosa, L. SO-22 Gut microbiome composition as predictor of the efficacy of adding atezolizumab to first-line FOLFOXIRI plus bevacizumab in metastatic colorectal cancer: A translational analysis of the AtezoTRIBE study. https://doi.org/10.1016/j.annonc.2023.04.494